Based on Your Reading:
Get Your Free Mesothelioma Guide

Find a Top Mesothelioma Doctor

Access Help Paying for Treatment

The primary goals of treatment for asbestos-related lung cancer are to remove or kill cancer cells to prevent the spread of cells and tumors and alleviate cancer symptoms and pain. Many types of lung cancer cannot be cured with available treatments, so a major focus of therapy is lessening symptoms to improve the patient's quality of life and survival rate.
Written by Suzanne Dixon, MPH, MS, RDN • Edited By Walter Pacheco • Medically Reviewed By Dr. Andrea Wolf
The Mesothelioma Center at Asbestos.com has provided patients and their loved ones the most updated and reliable information on mesothelioma and asbestos exposure since 2006.
Our team of Patient Advocates includes a medical doctor, a registered nurse, health services administrators, veterans, VA-accredited Claims Agents, an oncology patient navigator and hospice care expert. Their combined expertise means we help any mesothelioma patient or loved one through every step of their cancer journey.
More than 30 contributors, including mesothelioma doctors, survivors, health care professionals and other experts, have peer-reviewed our website and written unique research-driven articles to ensure you get the highest-quality medical and health information.
My family has only the highest compliment for the assistance and support that we received from The Mesothelioma Center. This is a staff of compassionate and knowledgeable individuals who respect what your family is experiencing and who go the extra mile to make an unfortunate diagnosis less stressful. Information and assistance were provided by The Mesothelioma Center at no cost to our family.LashawnMesothelioma patient’s daughter


Dixon, S. (2024, January 16). Asbestos-Related Lung Cancer Treatment. Asbestos.com. Retrieved April 16, 2024, from https://www.asbestos.com/cancer/lung-cancer/treatment/
Dixon, Suzanne. "Asbestos-Related Lung Cancer Treatment." Asbestos.com, 16 Jan 2024, https://www.asbestos.com/cancer/lung-cancer/treatment/.
Dixon, Suzanne. "Asbestos-Related Lung Cancer Treatment." Asbestos.com. Last modified January 16, 2024. https://www.asbestos.com/cancer/lung-cancer/treatment/.
Treatment can involve various forms of surgery, chemotherapy and radiation. When lung cancer is diagnosed, your doctor will explain the tumor’s histological type and assign it a stage. There are two main types of lung cancer — small cell and non-small cell.
Because small cell and non-small cell lung cancers grow, spread and react to treatments differently, your lung cancer’s histological type has a crucial impact on your treatment and outlook.
Exposure to asbestos is strongly associated with causing lung cancer, mesothelioma and several other severe respiratory diseases. Asbestos is the most common occupational risk factor for lung cancer, and workplace exposure significantly increases the chance of developing the disease.
Many times, treatment options will be limited by the stage of the patient’s cancer. Lung cancer spreads to the lymph nodes and distant organs as it progresses, which makes treatment increasingly difficult. Those diagnosed in the earliest stages of disease have the most treatment options and experience the greatest survival rates.
Non-small cell lung cancers are commonly classified with a four-stage system. A higher stage indicates more advanced disease.
Small cell lung cancer is staged using a two-stage system instead: Limited stage or extensive stage. In limited stage, the cancer is only found in one lung and possibly nearby lymph nodes. In extensive stage, the tumor has spread to the opposite lung or to other organs
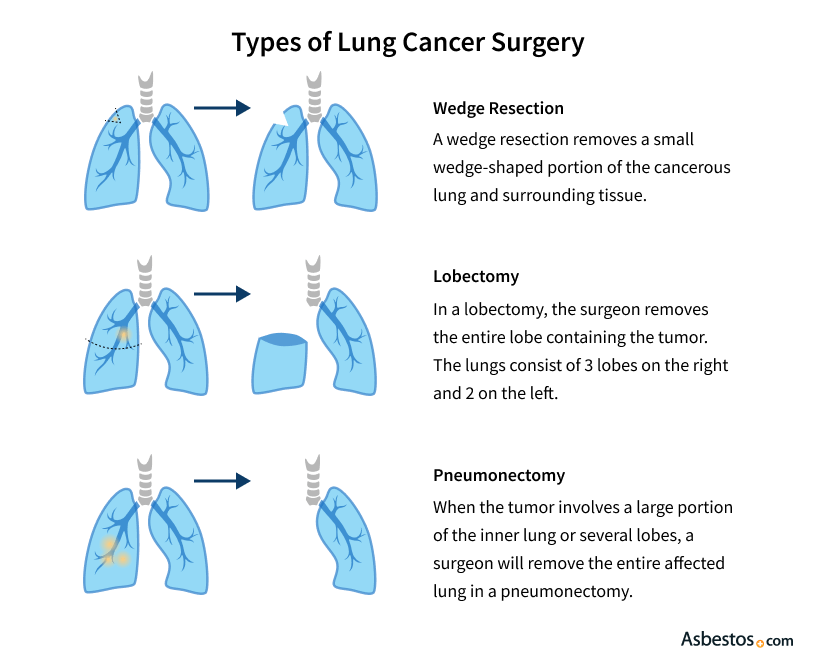
The ideal goal of surgery is to remove a tumor and nearby cancerous tissue, thus completely eliminating the disease. The extent of tissue removal varies depending on the tumor’s size, its location and how far the cancer has spread. Doctors also consider pre-existing conditions, such as heart disease, which could make a patient ineligible for surgery.
If the cancer is found in an early stage when spread is limited, curative surgery is preferred for its statistically high success rates. The majority of cases, however, involve advanced-stage cancer where a cure is unlikely. In this case, doctors perform palliative treatments that make symptoms more bearable while improving the patient’s outlook.
Doctors will look at the cancer’s histological type and extent of spreading before recommending surgery as a curative treatment option. If tumor growth is causing pain or undesirable symptoms, palliative surgery may be performed.
Get Your Free Mesothelioma Guide

Find a Top Mesothelioma Doctor

Access Help Paying for Treatment

In most cases, non-small cell lung cancers are removed through lobectomy. If the patient has poor lung function, however, doctors may remove only a small wedge of the lung via surgical resection.
Small cell lung cancer spreads much more aggressively than non-small cell, making surgery an option only in a few special cases. Although surgical treatment for small cell is rare, studies have reported positive results for the small percentage of patients with very limited disease.
When there is clear evidence that lung cancer has spread from the initial tumor, chemotherapy is recommended. This treatment is typically not curative for lung cancer, but has been known to reduce the size of tumors and kill cancer cells that have spread to the lymph nodes. For patients, this usually translates to a longer, more comfortable life.
Whether taken intravenously or in pill form, chemotherapy drugs target rapidly dividing cells. This kills cancer cells, but can also affect normal healthy cells including hair follicles, red and white blood cells and the cells that line the stomach. Because nearly half of all patients that have a tumor surgically removed will experience relapse, about 80 percent of all lung cancer patients are considered for chemotherapy during the course of their treatment.
In the earliest stages of non-small cell lung cancer, chemotherapy is sometimes given before surgery to reduce tumor size and eliminate early spreading. Doctors call this approach neoadjuvant chemotherapy. For patients with limited lymph node involvement, chemotherapy can also be given post-surgery to kill any remaining cancer cells. This is known as adjuvant chemotherapy and helps prevent the chance of cancer recurrence.
For later stage cancers when surgery is no longer an option, chemotherapy is often administered with simultaneous radiation therapy. Known as combined chemoradiation therapy, this option often boasts survival rates higher than either treatment given alone or one after the other. This treatment is common if the cancer has spread to the mediastinal lymph nodes, which are located outside of the lung near the trachea and esophagus.
For early-stage small cell lung cancer patients in otherwise good health, doctors recommend combined chemoradiation therapy. Small cell cancers are highly responsive to chemotherapy, and survival is significantly improved when it is combined with early radiation therapy.
Once the cancer enters the extensive stage and spreads to distant organs, doctors typically prescribe a platinum-based chemotherapy regimen. This will involve platinum containing drugs like cisplatin or carboplatin with one or more additional chemotherapy drugs.
When lung cancer patients are not eligible for surgery, radiation is often recommended. Radiation therapy uses high-energy targeted radiation to stop cancerous cell division and reduce the size of tumors. The amount of radiation administered is thousands of times greater than the amount used in X-ray imaging, but treatment is divided into doses to limit the damage done to healthy tissues.
Like surgery, radiation therapy is a local treatment that only affects cells in the treatment area. Response rates for radiation therapy are significantly high, but relapse is common so it is more often used as a palliative treatment. In this case, radiation is administered in small doses to lessen pain in areas where cancer has spread, such as the bones. It can also be given to prevent or treat lung cancers that spread to the brain.
For small cell lung cancer, radiation therapy is much less effective – especially if spreading to distant organs has occurred. The radiation can help with local control, but does nothing for small cell lung cancer’s primary threat of aggressive spreading.
While surgery, chemotherapy and radiation therapy are longtime pillars of lung cancer treatment, doctors are constantly conducting clinical trials to test new drug combinations. The primary goal is to improve current success rates while minimizing undesirable side effects. Many of the experimental lung cancer treatments described below are also used to treat mesothelioma, a rare asbestos-related cancer that affects the lining of the lungs. Clinical trials for these treatments will often accept both lung cancer and mesothelioma patients.
Targeted therapies prevent lung cancer from growing and spreading by interfering with specific molecules that control tumor growth, and these therapies normally have no negative effects on healthy cells. One FDA-approved targeted therapy is Avastin, an anti-angiogenesis drug. Avastin interferes with a crucial step in angiogenesis that stimulates the growth of blood vessels. Without a fresh supply of oxygen and nutrients supplied by the blood, tumors cannot grow past a small size.
Recent advancements in the understanding and manipulation of the immune system have allowed the development of immune checkpoint inhibitors such as nivolumab and pembrolizumab. These agents take advantage of the growth regulation of the cells and the immune system and have shown very promising results.
A 2021 study reported positive results combining photodynamic therapy with chemotherapy for lung cancer. Researchers reported improved disease control, reduced treatment resistance and increased overall effectiveness in cancer reduction compared to conventional options.
Gene therapy advances have opened the possibility of altering a person’s genetic material to fight or prevent cancer. In gene therapy, doctors introduce genetic material into a patient’s cells to fight disease. Several approaches are being tested in clinical trials.
The following examples of treatments are experimental, but may become commonplace if they prove to be safe and effective in ongoing clinical trials:

If you have been diagnosed with asbestos-related lung cancer, you likely will be treated by more than one doctor. Leading cancer facilities recommend a multidisciplinary approach to treatment, meaning several doctors specializing in different areas will work together to treat one patient. Some of the specialists who help formulate your treatment strategy and who execute it include:
Because lung cancer is so prevalent — the second-most diagnosed cancer in the United States — there are no shortage of doctors who treat it. The number of doctors who specialize in asbestos-related lung diseases is much smaller. Treating asbestos lung cancer comes with a special set of circumstances and challenges. Here is a breakdown by region of some treatment centers and specialists who tackle asbestos-related lung diseases.
In addition to New York state, the northeastern corridor is home to a number of regarded doctors who treat asbestos lung cancer and other asbestos-related diseases.
Bueno is the associate chief of thoracic surgery at Brigham and Women’s Hospital in Boston. His research has centered on developing new ways to diagnose and treat most thoracic cancers, including lung cancer. He has many local, national and international collaborators for his research, developed through years of work. He trained at Harvard Medical School, did a cardiothoracic residency at Massachusetts General and rejoined Brigham and Women’s in 1996 to establish a thoracic surgery practice and research laboratory.
Chairman of the University of Pittsburgh Medical Center Lung and Esophageal Surgery Institute, Luketich champions the multi-disciplinary management of lung cancer and benign esophageal disease. He specializes in all areas of thoracic oncology, and is the co-director of the Lung Cancer Center at UPMC. He is board certified in both thoracic and general surgery, having worked at both the Cleveland Clinic in Ohio and at the Hospital of the University of Pennsylvania, as well at Memorial Sloan Kettering in New York.
An increasing number of specialists who treat his disease are cropping up in the Southeastern part of the United States.
Baxter is an assistant professor of surgery at the University of Miami Sylvester Comprehensive Cancer Center. She is the medical director of the Lung Cancer Screening Program with strong clinical interests in the early detection and treatment of the disease. She is involved in the surgical management of a wide range of thoracic diseases, including tracheal and bronchoplastic procedures, esophageal cancer and lung cancer. She has extensive experience with minimally invasive thoracic surgery for both malignant and benign pleural diseases.
Mazzone is the director of both the Lung Cancer Program for the Respiratory Institute and the director of the Pulmonary Rehabilitation Program at the Cleveland Clinic. His treatment interests include lung cancer, lung nodules and intensive care medicine. His research has focused on lung physiology, lung cancer screening and lung cancer diagnostics. He did his fellowship in Pulmonary and Critical Care Medicine in Cleveland. His specialty interests include acute respiratory distress syndrome, asthma, pneumonia and lung cancer.
The American Southwest is home to a number of qualified surgeons who treat asbestos lung cancer.
A thoracic surgeon at the University of Texas MD Anderson Cancer Center, Rice is a pioneer in the field of minimally invasive methods to deal with thoracic tumors. Originally from Ireland, he was one of the first surgeons in the United States to be trained in endobronchial ultrasound for the staging of lung cancer. He focuses on a high volume of minimally invasive lobectomies and esophagectomies for lung and esophageal cancer.
At the Texas A&M Health Science Center College of Medicine, Smythe focused his patient care on chest wall tumors, advanced lung cancer, and benign lung disease. He is chairman of the department of surgery at Scott and White Memorial Hospital. His specialties include cardiothoracic surgery, thoracic surgery and general surgery. During his residency at the University of Pennsylvania, he was the lead author on the first paper describing the use of adenoviral based gene therapy to treat cancer models in the laboratory.
California is home to a number of highly regarded lung cancer treatment centers and doctors.
Shrager is a professor in the Stanford University School of Medicine Thoracic Surgery Division. He is on the editorial board of the Annals of Thoracic Surgery. Although he practices all aspects of thoracic surgery, his special interests include lung cancer, surgery for emphysema and mediastinal diseases. He is a proponent of minimally invasive procedures, including VATS (thoracoscopic) lobectomy for early-stage lung cancer. In research, he has focused on the respiratory muscles to various diseases.
Gandara is director of clinical research for thoracic oncology at the University of California Davis Cancer Center. He is a leader in developmental therapeutics for new anticancer agents. His clinical research and modeling in lung cancer has been rewarded by the National Cancer Institute, where he is the principal investigator in the Early Therapeutics Program. He leads a multi-specialty team in the Southwest Oncology Group that studies improving therapies and predictive biomarkers for lung cancer. He was awarded the prestigious Addario Lectureships Award for his innovative lung cancer research, and was featured prominently on a PBS Newshour show earlier this year on the “War on Cancer,” which was declared 40 years ago by President Richard Nixon.
Like the South, the Northwestern part of the United States is seeing a growth in the number of doctors who treat asbestos lung cancer and mesothelioma.
Vallieres is surgical director of the Swedish Cancer Institute Lung Cancer Program. His clinical interests include lung cancer, pleural diseases, chest wall tumors, mediastinal masses, and esophageal achalasia. He specializes in both robotic and thoracic surgery. His theory, on the Swedish website, is that if you provide the right treatment for the right stage of lung cancer, you should expect better results. He has written several book chapters and done videos on non-small cell lung cancer, including the role of surgery, and the management of stage 3 cancers.
The Hematology/Medical Oncology Division Chief of the Oregon Health and Science University, Sandler is a nationally-renowned lung cancer specialist. He is the principal investigator or co-principal investigator of several combined modality therapies for both small and non-small lung cancer. Before joining OHSU, he was the medical director of thoracic oncology at Vanderbilt University. He serves on the editorial board for both Clinical Lung Cancer and the Japanese Journal of Clinical Oncology. One of his specialties is cancer and blood disorders. He is the author of more than 200 published articles covering clinical activity of novel target agents, with a particular emphasis on lung cancer.
Your web browser is no longer supported by Microsoft. Update your browser for more security, speed and compatibility.
If you are looking for mesothelioma support, please contact our Patient Advocates at (855) 404-4592
