Based on Your Reading:
Get Your Free Mesothelioma Guide

Find a Top Mesothelioma Doctor

Access Help Paying for Treatment

Numerous environmental factors such as asbestos, silica dust, coal dust, cotton dust, and hard metal dusts can cause several forms of interstitial lung disease (ILD). Diseases such as lupus, rheumatoid arthritis, sarcoidosis, and other connective tissue and blood-related disorders can also cause ILD. It is sometimes caused by certain medications and infections, including pneumonia and cytomegalovirus. The form of interstitial lung disease caused by asbestos is called asbestosis. Asbestosis is also known as pulmonary fibrosis and interstitial pneumonitis.
Written by Karen Selby, RN • Edited By Walter Pacheco • Medically Reviewed By Dr. Rupesh Kotecha
The Mesothelioma Center at Asbestos.com has provided patients and their loved ones the most updated and reliable information on mesothelioma and asbestos exposure since 2006.
Our team of Patient Advocates includes a medical doctor, a registered nurse, health services administrators, veterans, VA-accredited Claims Agents, an oncology patient navigator and hospice care expert. Their combined expertise means we help any mesothelioma patient or loved one through every step of their cancer journey.
More than 30 contributors, including mesothelioma doctors, survivors, health care professionals and other experts, have peer-reviewed our website and written unique research-driven articles to ensure you get the highest-quality medical and health information.
My family has only the highest compliment for the assistance and support that we received from The Mesothelioma Center. This is a staff of compassionate and knowledgeable individuals who respect what your family is experiencing and who go the extra mile to make an unfortunate diagnosis less stressful. Information and assistance were provided by The Mesothelioma Center at no cost to our family.LashawnMesothelioma patient’s daughter


Selby, K. (2024, February 2). Interstitial Lung Disease & Asbestos. Asbestos.com. Retrieved April 16, 2024, from https://www.asbestos.com/mesothelioma/interstitial-lung-disease/
Selby, Karen. "Interstitial Lung Disease & Asbestos." Asbestos.com, 2 Feb 2024, https://www.asbestos.com/mesothelioma/interstitial-lung-disease/.
Selby, Karen. "Interstitial Lung Disease & Asbestos." Asbestos.com. Last modified February 2, 2024. https://www.asbestos.com/mesothelioma/interstitial-lung-disease/.
Interstitial lung disease is a term for a group of diseases that cause scar tissue. The respiratory system clears foreign matter, such as dust, from the body. In some cases, the repair process often leads to scarring and injury when the body responds to this type of injury. Asbestos fibers are especially challenging for the lungs to expel.
The term interstitial pneumonitis refers to inflammation. Unlike pneumonia, it is not caused by an infection. Asbestos exposure causes a type of interstitial pneumonitis known as asbestosis.
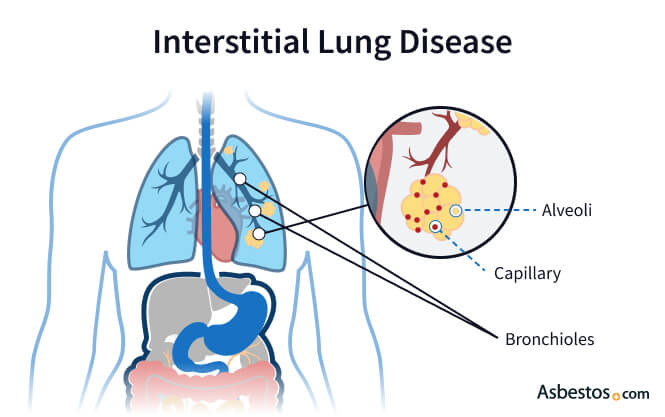
This disease is an inflammation of the lungs that causes severe scarring. Bronchioles are small airways within your lungs. They contain clusters of air sacs called alveoli. The interstitium is the tissue that lines and supports the alveoli.
Inflammation causes thickening and scarring of the interstitium. The air sacs also become thicker and begin to lose elasticity. This causes a loss of their ability to put oxygen into the blood and remove carbon dioxide.
Asbestosis is a progressive disease, meaning scarring continues, and symptoms worsen with time. Interstitial lung disease from asbestos exposure can take 10 to 30 years to appear. Asbestosis scarring slows when asbestos exposure ends. Lung damage caused by asbestos exposure is irreversible. Doctors can use palliative treatments to relieve symptoms.
There are a number of different types of ILD in addition to asbestosis.
The symptoms of asbestosis and other interstitial lung diseases are similar to the symptoms of other lung conditions such as COPD and asthma. Unfortunately, by the time the symptoms appear, permanent lung damage has already occurred.
The following symptoms are the most common signs of interstitial lung disease:
The similarity of ILD symptoms to other lung conditions can often make diagnosis difficult. Doctors use chest X-rays, CT scans, and pulmonary function tests to diagnose these diseases.
Chest X-rays rule out other lung conditions, such as a collapsed lung or emphysema. They cannot diagnose interstitial lung disease alone. A high-resolution computerized tomography scan (HRCT) can produce detailed images of the lungs. HRCTs are very helpful in the diagnosis process.
Doctors may also use pulmonary function and exercise tests to determine lung capacity. A simple lung capacity test requires a patient to blow into a spirometer, an instrument used to measure lung capacity. A doctor may also evaluate a patient’s lung capacity while riding a stationary bike or walking on a treadmill.
An oximetry test may be used to monitor oxygen saturation in the blood, which can help track the progression of the disease. In advanced cases, blood oxygen levels drop.
An echocardiogram is sometimes used to determine the amount of pressure placed around the heart. This test uses sound waves to produce images of the heart and can help visualize where the pressure originates.
Sometimes a tissue sample from the lungs is needed before a definite diagnosis can be made. This can be obtained with a bronchoscopy (transbronchial biopsy) or bronchoalveolar lavage. The doctor will insert a fiber-optic, flexible tube (bronchoscope) for a transbronchial biopsy. The scope goes through the mouth and lungs to collect tiny tissue samples.
A bronchoalveolar lavage is often used to check the progress of interstitial lung disease in someone with the condition. A sample requires a bronchoscope to inject a saline solution (salt water) into the lung. The solution captures cells from the air sacs. The doctor then immediately suctioned the saline out from the lung. The fluid goes to a lab for study and diagnosis.
Occasionally, a surgical lung biopsy is necessary to obtain a definite diagnosis. The surgeon will make a small incision between the ribs and insert a tube with a camera on the end (an endoscope) to view the lungs. This is also called video-assisted thoracoscopic surgery or VATS. Through another small incision, the surgeon will insert an instrument to obtain a lung tissue sample.
Get Your Free Mesothelioma Guide

Find a Top Mesothelioma Doctor

Access Help Paying for Treatment

Treatment relieves symptoms and prevents complications like high blood pressure and heart disease. Oxygen may help a patient experiencing shortness of breath. Anti-inflammatory medications such as corticosteroids may also improve symptoms.
Anti-fibrotic medication, such as pirfenidone, can reduce the rate of progression. A class of drugs called tyrosine kinase inhibitors can reduce fibrosis progression. One such drug used to treat idiopathic pulmonary fibrosis is nintedanib.
Pulmonary rehabilitation is an option for many people with ILD. However, it is generally underused because few physicians know that it benefits ILD patients and thus don’t know to recommend the therapy. Pulmonary rehabilitation involves working with a trained therapist who teaches breathing exercises and techniques to improve lung function.
A person with fluid in their lungs may have a doctor drain any excess fluid to help them breathe easier. A lung transplant may be recommended in rare cases where the lungs are extremely damaged. Fortunately, most people do not require such extreme treatments for asbestosis.
A doctor will also advise a patient to take precautions to avoid the flu since people with interstitial lung disease are prone to complications from any respiratory infection. Your health provider may suggest vaccination against the flu and against pneumonia. Regular monitoring of your condition can also help prevent any other complications.
The complications of asbestosis and other interstitial lung conditions can be life-threatening. Pulmonary hypertension (high blood pressure in the lungs) is a serious problem with these diseases. Pulmonary hypertension occurs when the blood vessels in the alveoli become damaged by scarring. Medicines that relax or expand the blood vessels can treat this problem. Doctors may also use blood thinners to prevent blood clots in these conditions.
People with asbestosis may also experience other complications. The Mayo Clinic reports that people with asbestosis who smoke have a greatly increased risk of developing lung cancer. Quitting smoking can reduce your risk of lung cancer and improve your overall lung function and quality of life.
Additional lung damage, such as pleural plaques and pleural effusions, may also occur if you have asbestosis. Pleural plaques are calcium deposits on the pleura, which is the lining of the lungs. Pleural effusions are abnormal accumulations of fluid between the membranes of the lungs. Although pleural effusions are benign, they indicate that a person has been exposed to asbestos or another hazardous material. The amount of asbestos exposure necessary to cause asbestosis can also cause malignant mesothelioma.
The severity of asbestosis depends on the length and amount of asbestos exposure. Other factors include your general physical health and lifestyle choices such as smoking. People who smoke while exposed to asbestos are especially likely to develop asbestosis.
Because asbestosis is not cancer, people can live many years with the disease. If detected and treated early, asbestosis may not lead to severe complications.
Reducing or eliminating asbestos exposure is the best way to prevent asbestosis. Since the late 1970s, many regulations have protected workers from asbestos exposure. Homes built before or during the 1980s may contain asbestos-containing construction materials. As long as these products are in good condition, they are safe.
Asbestos exposure can occur when residents or workers remove or disturb asbestos-containing materials. Consult an asbestos-abatement professional before you begin this type of project.
Your web browser is no longer supported by Microsoft. Update your browser for more security, speed and compatibility.
If you are looking for mesothelioma support, please contact our Patient Advocates at (855) 404-4592
