Based on Your Reading:
Get a Mesothelioma Treatment Guide

Find a Top Mesothelioma Doctor

Access Help Paying for Treatment

Paclitaxel is a drug used experimentally in mesothelioma treatment. It may be an effective substitute for pemetrexed (Alimta) in pleural mesothelioma chemotherapy. Some peritoneal mesothelioma patients have benefited from follow-up paclitaxel treatments after surgery.
Written by Karen Selby, RN • Edited By Walter Pacheco • Medically Reviewed By Dr. Rupesh Kotecha
The Mesothelioma Center at Asbestos.com has provided patients and their loved ones the most updated and reliable information on mesothelioma and asbestos exposure since 2006.
Our team of Patient Advocates includes a medical doctor, a registered nurse, health services administrators, veterans, VA-accredited Claims Agents, an oncology patient navigator and hospice care expert. Their combined expertise means we help any mesothelioma patient or loved one through every step of their cancer journey.
More than 30 contributors, including mesothelioma doctors, survivors, health care professionals and other experts, have peer-reviewed our website and written unique research-driven articles to ensure you get the highest-quality medical and health information.
My family has only the highest compliment for the assistance and support that we received from The Mesothelioma Center. This is a staff of compassionate and knowledgeable individuals who respect what your family is experiencing and who go the extra mile to make an unfortunate diagnosis less stressful. Information and assistance were provided by The Mesothelioma Center at no cost to our family.LashawnMesothelioma patient’s daughter


Selby, K. (2024, February 2). Paclitaxel (Taxol). Asbestos.com. Retrieved April 18, 2024, from https://www.asbestos.com/treatment/drugs/paclitaxel/
Selby, Karen. "Paclitaxel (Taxol)." Asbestos.com, 2 Feb 2024, https://www.asbestos.com/treatment/drugs/paclitaxel/.
Selby, Karen. "Paclitaxel (Taxol)." Asbestos.com. Last modified February 2, 2024. https://www.asbestos.com/treatment/drugs/paclitaxel/.
Paclitaxel is approved by the U.S. Food and Drug Administration (FDA) for use against breast cancer, non-small cell lung cancer, ovarian cancer, AIDS-related Kaposi’s sarcoma and pancreatic cancer.
Doctors also use it as an experimental or off-label treatment for bladder cancer, esophageal cancer, melanoma, prostate cancer and mesothelioma. Paclitaxel is commonly given in combination with cisplatin or carboplatin.
A 2021 clinical research study concluded that large doses of intraperitoneal paclitaxel, up to 120 mg every month or 60 mg weekly, can be combined with cisplatin and other systemic agents with minimal or no additional hematologic toxicity.
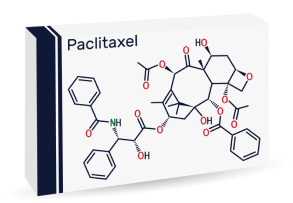
Paclitaxel is an antimicrotubule agent. Microtubules are an essential part of the process by which cells divide. Paclitaxel binds to proteins in cell microtubules, which forces cells to stop dividing. Since cancer cells divide rapidly, their microtubules are a good target for chemotherapy.
This drug dates back to the late 1960s when it was discovered in the bark of the Pacific yew tree. Researchers recognized its potential as an anti-cancer agent, but its natural scarcity made it challenging to market.
More than 20 years later, researchers found a way to produce paclitaxel synthetically. Bristol-Myers Squibb began marketing it as Taxol.
In 2005, the FDA approved a new type of drug called nanoparticle albumin-bound paclitaxel, or nab-paclitaxel. In this formulation, the drug is contained in tiny particles of protein. This improves drug delivery and reduces side effects. Celgene Corporation markets nab-paclitaxel as Abraxane.
| Name | Taxol, Abraxane |
| Manufacturer | Bristol-Myers Squibb, Celgene |
| Medical Code | J9267 |
| Dosage | 135 mg/m² |
| Administration Route | Intravenous or intraperitoneal |
| Active Ingredient | Paclitaxel |
| Drug Class | Antineoplastic agent, antimicrotubule agent |
| Related Drug | Docetaxel |
| Alternate Names | Anzatax, Asotax, Bristaxol, Onxol, Praxel |
| Interacting Drug | Adenovirus types 4 and 7 live, antihistamines, apalutamide, eluxadoline, idarubicin, idelalisib, influenza virus vaccine trivalent, ivacaftor, nefazodone, opiates, palifermin, quinidine |
| Medical Studies | Long-term regional chemotherapy for patients with epithelial malignant peritoneal mesothelioma results in improved survival |
| FDA Warning | Skin problems, hives, acute allergic reaction characterized by breathing difficulty and low blood pressure |
Get a Mesothelioma Treatment Guide

Find a Top Mesothelioma Doctor

Access Help Paying for Treatment

In the 1990s, studies of paclitaxel (Taxol) as a single agent for pleural mesothelioma showed slight effectiveness. Now researchers are testing nab-paclitaxel (Abraxane) in combination with other drugs.
A 2016 study published in Respirology Case Reports described one medical team’s success in substituting nab-paclitaxel for pemetrexed.
Standard chemotherapy for mesothelioma combines pemetrexed with cisplatin or carboplatin, but pemetrexed is too toxic for some patients. In the case report, a pleural mesothelioma patient responded well to nab-paclitaxel with carboplatin after standard chemotherapy had failed.
In 2017, Clinical Cancer Research published the results of a laboratory experiment using mesothelioma cells. The researchers combined nab-paclitaxel with an experimental immunotoxin called RG7787, with good results.
That same year, Biomedicine & Pharmacotherapy reported on a novel drug delivery method for mesothelioma. The laboratory experiment involved loading paclitaxel into a particular cell type to help the drug reach cancer cells.
Paclitaxel also shows promise for peritoneal mesothelioma, according to a 2017 European Journal of Surgical Oncology review. The review was co-authored by Dr. Paul Sugarbaker.
Sugarbaker helped pioneer the technique of rinsing a patient’s abdomen with chemotherapy during surgery. This procedure is called hyperthermic intraperitoneal chemotherapy (HIPEC). It is associated with much longer survival times for peritoneal mesothelioma patients.
In the 2017 review, Sugarbaker’s team reported that outcomes are the best for patients who also get long-term paclitaxel. In these follow-up treatments, the drug is delivered to the abdomen to prevent cancer reoccurrence.
Like most chemotherapy drugs, paclitaxel damages healthy and cancer cells. Side effects are usually worst about 15 to 21 days after treatment.
Your web browser is no longer supported by Microsoft. Update your browser for more security, speed and compatibility.
If you are looking for mesothelioma support, please contact our Patient Advocates at (855) 404-4592
