Pulmonologist Dr. Edmund Moon on Mesothelioma Immunotherapy
In recent years, it has become increasingly clear that immunotherapy may be the most crucial advancement in cancer research perhaps ever.
Early in my medical career, I was not initially interested in cancer research. During my interventional pulmonary fellowship training at the University of Pennsylvania, I developed a meaningful and productive partnership with the thoracic oncology research lab.
Simultaneously, a new T-cell immunotherapy initiative at UPenn was gaining popularity. It was the perfect time to transition into a cancer research career. Looking ahead, I am excited about the potential of immunotherapy and how it can change the course of mesothelioma treatment.
Recent Immunotherapy Research Shows Promise
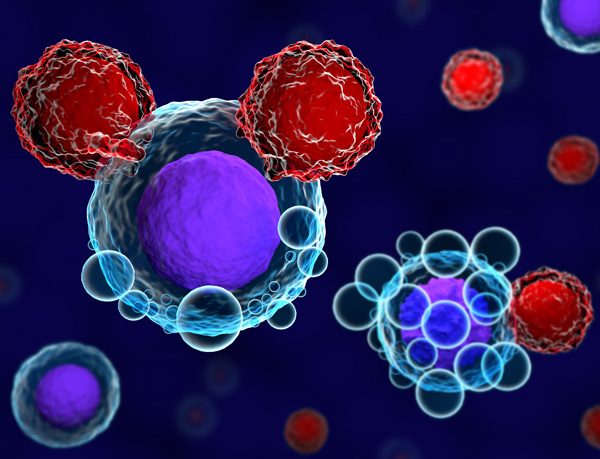
Historically, T-cell immunotherapy has proven to be very successful in treating hematologic cancers such as leukemia. When adopting the technology for solid cancers, such as lung cancer and mesothelioma, overcoming certain obstacles requires us to develop novel approaches.
One of the first steps in this process is characterizing the tumor microenvironment. In other words, we must identify how tumor cells interact with our body and immune system. This area is one of my primary areas of research.
In 2019, I published several papers on the role of unique T-cell variants, immune cells that help fight infection. When modified in a laboratory, scientists can program these cells to identify cancer targets such as mesothelin, a protein present on mesothelioma cells.
Earlier this year, my colleagues and I published research on why some lung cancer patients may not respond to T-cell immunotherapy. Immune checkpoint treatment relies on removing the blocks that prevent T cells from identifying and attacking solid tumors. This has worked in certain settings. However, in many cases, tumor cells can defend themselves by compensating with other inhibitory molecules.
Our research discovered that combining therapies that blocked PD1 and TIM3 checkpoints resulted in greater tumor control than inhibiting PD1 alone. These results will help lead to more discoveries of the optimal combination of immunotherapies for mesothelioma patients.
There is still much we need to learn about our immune system and how it interacts with different cancers, but identifying potential new treatments is one of the most exciting parts of my research career.
Benefits of Immunotherapy for Mesothelioma Patients
Many cancer patients are choosing immunotherapy as part of their multimodal treatment plan. Clinical trials have shown that these drugs successfully boost the immune system to shrink tumors and prevent regrowth.
The U.S. Food and Drug Administration has approved two immune checkpoint inhibitor therapies for mesothelioma patients. The first, Keytruda, also known as pembrolizumab, has been a valuable option for lung cancer patients and is now available as a second-line treatment for mesothelioma patients.
The second option, approved in October 2020, is a combination therapy of Opdivo and Yervoy, known as nivolumab and ipilimumab, respectively. The FDA previously approved this treatment as first-line therapy for metastatic non-small cell lung cancer. This type of combination immunotherapy is key to unlocking the anti-tumor benefits of the immune system.
T cells are essential for identifying and destroying tumor cells. Opdivo works by helping T cells discover the mesothelioma tumor, and Yervoy activates and proliferates T cells so that there is enough in the circulating blood.
An experimental approach in engineering T cells against cancer is CAR T-cell therapy. It is a type of adoptive cell transfer, an area of my work that involves genetically modifying receptors on the surface of T cells. We can manipulate those receptors to “see” and connect with antigen proteins specific to the cancers in individual patients.
We replicate these T cells in a lab and then deliver them back to the patient. The initial results for mesothelioma are promising, but more research is needed to find the best targets on the surface of solid tumors.
Overall, immunotherapy is a critical new treatment method for mesothelioma patients, and I am excited to be a part of its future. Working with an energetic and internationally renowned team at UPenn has been a motivational experience. As research continues in this promising new field, I expect we will soon see unprecedented advances against this terrible disease.