
Get a mesothelioma treatment care kit filled with thoughtful items to bring comfort and encouragement while undergoing treatment.
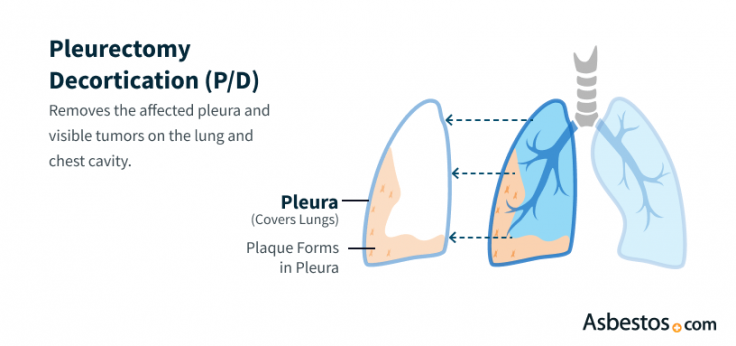
Get Your Free KitPleurectomy and decortication (P/D) is a surgery for pleural mesothelioma that removes the lung lining and visible tumors. It’s often chosen because it leaves the lung in place, helping people breathe more easily and feel better during recovery.
Pleurectomy/decortication (P/D) is a surgery for pleural mesothelioma, the most common type of mesothelioma. It removes the lining of the lung and visible tumors but leaves the lung itself in place. This can ease symptoms, improve breathing and help people live longer.
Key Facts About Mesothelioma Pleurectomy With Decortication
P/D is often combined with chemotherapy, radiation or immunotherapy to destroy any mesothelioma cells left behind. This multimodal approach can help extend survival and lower the risk of the cancer returning.
Because the lung is left in place, many people with mesothelioma can breathe more easily after surgery and recover with less impact on daily life. P/D may be a good option for those looking to manage symptoms while staying as active as possible.
There are 2 main types of pleurectomy/decortication surgery for pleural mesothelioma. Both aim to remove as much cancer as possible while helping you keep your strength and lung function. The difference is in how much tissue is removed based on how far the cancer has spread.
P/D Surgery Options
Doctors use imaging and other tests to see how far the cancer has spread and decide which surgery is right for you. Your surgeon will talk with you about your options, aiming to remove as much mesothelioma as possible while helping you feel better, breathe easier and live longer.
A thoracic surgeon performs pleurectomy/decortication in a hospital under general anesthesia. It’s an inpatient procedure, and most people stay in the hospital for several days to recover. In the first step, surgeons remove the pleural lining from the chest wall. In the second, they focus on tumors and affected tissue on the surface of the lung.
Pleural mesothelioma survivor Joe Barna credits P/D surgery for his success. He tells us, “I remember Dr. DaSilva going into surgery talking about my disease, in so many words saying, ‘We’re going to kick its ass.’ He just gave me such an incredibly positive feeling. My last checkup with him, he told me, ‘You don’t even need to be here.’”
To start the mesothelioma procedure, the surgical team positions you on your side. Your surgeon then makes a long incision along your back, called a thoracotomy, to open your chest cavity. This incision runs from near your spine down toward your lower ribs.
If mesothelioma has spread to the lower chest, a second incision may be needed. In some cases, the sixth rib is removed to create more space. Your surgeon removes your parietal pleura, the outer layer of the lung’s lining, along with any visible cancer on the chest wall lining, heart sac or diaphragm.
Once the pleurectomy is complete, your surgeon begins the second part of the procedure: removing visible mesothelioma tumors from the surface of your lung. In some cases, they gently scrape the lung to clear away any remaining cancer. When the cancer has been removed, the surgeon closes your incision with stitches.
“We’re finding that we’re able to remove all the tumor that’s visible,” Dr. Andrea Wolf, director of the New York Mesothelioma Program at Mount Sinai, tells us. “That’s why there’s been a shift toward doing this lung-sparing procedure more so than in decades past.”
Before finishing the surgery, the team seals blood vessels to prevent bleeding. Some surgeons may also use additional treatments during surgery. These include photodynamic therapy, heated chemotherapy solutions and experimental chemotherapy gels.

Get a mesothelioma treatment care kit filled with thoughtful items to bring comfort and encouragement while undergoing treatment.
Get Your Free KitBefore pleurectomy/decortication, your care team takes several important steps to get you ready for this mesothelioma surgery. These steps help doctors better understand your overall health and plan a safe and effective procedure. Knowing what to expect can help you feel more informed and in control.
What to Expect from Pleurectomy/Decortication Surgery
What to Expect from P/D Surgery and Recovery
I’d like to explain what a patient can can expect from a typical pleurrectomy decortication, at least from my experience over the last eleven years. And typically that means surgery starts usually in the morning, around eight in the morning, and it’s about four hour long surgery. We always put some type of device in called an epidural to help with your pain control for afterwards.
You’ll be on a ventilator, which is normal, meaning breathing on one side, the other side I’ll be operating on. I will peel off all that lining of the lung, and again, four hours, so say eight to twelve, You will then go to the ICU. Every patient goes to the ICU afterwards just to really get good monitoring of you, make sure that you recover.
You’re in the ICU for about two to three days, and then on average after that, the whole length of stay on the floor, the regular floor in the hospital, is about seven to eight days. I tell patients, tell everybody, it’s about on average a length of stay of ten to twelve days. From the time of surgery, from when you leave the hospital.
The majority of patients will be walking after surgery, be on pain medications, be eating, but the main thing that I always like to talk about and let patients know is that they’ll have a lot of tubes in. Everybody’s different. I put three to four tubes in, but most people put at least two tubes in.
These are chest tubes that’ll be on the side of draining fluid and air of where we took off that orange peel of the lung, the lung needs to recover and inflate. And so those tubes help with that, get rid of air, get rid of fluid to keep everything nice and clean in the chest. Those will stay in that whole time, and that’s the main reason why patients stay in the hospital.
It’s because the chest tubes, the lung need to heal. Pain starts to get better after the first week, But it’s really those chest tubes, the air leaking around the lung, takes about ten to twelve days. So then you go home.
Most patients go home. I would say more on the ten to fifteen percent depending on What you were like Before surgery, would go to maybe a rehab facility for a week or two and then home. Majority, eighty nine percent of my patients will go home, and I always talk to them about that.
And so they’ll go home, they won’t be driving, they’ll be eating, walking twenty minutes a day, stairs may be a little harder, and the majority will have a walker just for bracing themselves because it is such a, A fairly big incision, and you still have a little bit of pain and you’re recovering. So that’s the six week time period. After six weeks, the walker’s usually gone driving a little bit, being able to fly.
I usually like six weeks to fly. Those are the big things that people ask, or long road trips, things like that. After that, three months.
So that’s the next time period. After three months is when we’d say, k. You can pretty much do anything you want.
You’re not gonna hurt anything. And then that’s usually anywhere from two to three months after the surgery is when they’ll be well enough to start their therapy, some type of systemic therapy, which is usually chemotherapy, Two agents of chemotherapy. So they’re totally good by then.
Your weight will be back up. You’ll feel strong enough for that. That’s kind of the overall recovery period.
So if we were to rehash, I would say it’s in the three month ball six week to three month ballpark. And one other question that I get for patients in terms of what can I expect my functional capacity to be for like what it was before? I’d say on average we shoot for seventy five to eighty percent of your functional capacity of what you were like before.
I wouldn’t say you can expect every time or for all comers, you’re gonna be a hundred percent like you were before you never had mesothelioma. I think that’s a little bit on the less side. Certainly, I have patients that are functional, that go back, they work, they do everything, but they notice it.
They notice it. Right? They know, So, You know, in the two or three years out, they feel something or or whatnot.
It’s just not perfect. So really what I say is seventy five to eighty percent. But Driving, moving around, eating, going to dinner, still very, very doable and possible.
For whatever it’s worth, that’s what I think is still good considering we’re treating your cancer, but again, it’s something for you as the patient to remember that it’s very hard to say that you’re gonna be one hundred percent back to normal after the surgery and the chemotherapy and all the things that go through treatment.
Undergoing Pleurectomy/Decortication Surgery
The first treatment for the mesothelioma was a pleurectomy decortication, which is an operation. They cut through the middle of your back, between your ribs to the almost the middle of your front. It was supposed to be a eight inch incision, but it looks more like twelve. It, they had to remove a rib. They took the cancer that was collected around my the plural, lining of my lung and it was scraped off. I had six lymph nodes cut off. Two of them turned out also positive for mesothelioma. So I was pretty close to the stage where I was still a candidate to have the operation done, because it hadn’t, spread further.
Mesothelioma survivor describes her P/D experience
I knew that I would be in the hospital for, you know, at the very least a week. And that I was going to have radiation for five weeks after that. Doctor Cameron said you will probably be in pain for, like, a year. And he said, well, Kim, some patients, when they bend over, they get short of breath. Because I’m probably going to rearrange reconstruct your diaphragm. And so you might have that. You may have coughing. You may have increased flem and secretions. You may have shortness of breath, but you will be able to go back to work. And I said, really. And I said, okay. That sounds great to me. Jeanette came came with me. She stayed in the hospital, and my friend Stacy came. And my husband, Richard, they allowed the three to stay in the hospital room with me. My surgery ended up being about eight hours. I woke up. I remember going in, and I was nervous. You know, I thought, well, what if I don’t wake up? Prior to the surgery, had my will taken care of, my trust. I I kind of wrapped up those kind of legal issues. And, When I woke up, I remember thinking, I made it. I made it. I, you know, I knew that as a nurse, that there was a possibility that I I could maybe not make it through surgery, but I remember saying to my cousin who was there. It was the first face that I call. And I said, oh my gosh, Elaine, you’re here. I I made it. And really, after that, I thought, well, I don’t wanna say I was home free, but I thought, okay. Oh, you’re gonna be fine, Kim.
How to Prepare for P/D Surgery
Clear planning allows your medical team to perform surgery safely and address any concerns you may have ahead of time. Staying connected with your surgical team helps you feel supported every step of the way.
Most people stay in the hospital for about two weeks after pleurectomy/decortication for mesothelioma. During this time, doctors monitor your progress, manage any complications and begin therapies to support breathing and healing. Nurses and therapists may also begin teaching you exercises to support your recovery from surgery.
Once you return home, recovery continues over the next several weeks. Your care team will give you clear instructions, help coordinate follow-up care and may recommend additional support such as pulmonary rehabilitation. Staying involved in your care and attending follow-up appointments can make a meaningful difference in how you heal.
People in overall good health with an early-stage mesothelioma diagnosis may qualify for P/D. This lung-sparing procedure is most effective when the cancer is still confined to the chest, such as in stage 1 or 2 pleural mesothelioma. In these stages, surgery can often remove most or all visible tumor tissue.
Key Factors That Affect Eligibility for P/D Surgery
Not everyone diagnosed with mesothelioma will initially qualify for P/D surgery. But many people have discovered new options by getting second opinions and advocating for their care. Your doctor will carefully evaluate your overall health and cancer stage to determine if surgery is a good fit for you. If it’s not, they can help guide you to other mesothelioma treatment options tailored to your needs.

Kevin Hession
Mesothelioma Survivor Talks Life After Decortication Surgery
Kevin Hession underwent decortication surgery to remove all visible tumors in January 2022, about 5 months after being diagnosed with pleural mesothelioma. Kevin spoke with The Mesothelioma Center to share his experiences while recovering from surgery and to explain some lasting effects from the procedure.
Kevin Hession
P/D can help people with pleural mesothelioma live longer and breathe easier. Removing visible tumors while sparing the lung helps relieve symptoms and maintain lung function.
Doctors often recommend P/D when mesothelioma hasn’t invaded the lung itself. Research shows it offers positive outcomes with a low risk of serious complications.
Primary Advantages of P/D
Some clinical trials are testing ways to enhance results. For example, Dana-Farber is studying P/D with intensity-modulated radiation therapy. A 2023 trial questioned whether surgery plus chemo offers better outcomes than chemo alone. Patients should explore all mesothelioma treatment options with their mesothelioma care team, and ask whether P/D is right for them.

Hear from one of the nation’s top thoracic surgeons about how surgery can be effective for certain people with pleural mesothelioma.
Reserve Your SpotCommon risks of P/D for mesothelioma include infection, bleeding, fatigue and breathing problems. Serious complications are rare, but every surgery comes with some risk. Knowing what to expect can help you talk with your doctor and feel more prepared.
Potential Surgical Risks
Your doctor will watch for signs of complications and help manage any symptoms during recovery. Sharing your concerns and asking questions before surgery can help you feel more confident about the care you’ll receive.
Many doctors prefer pleurectomy/decortication because it removes cancer but keeps the lung. It can help some people with pleural mesothelioma feel better and live longer. Your care team will decide if it’s the best surgery for you based on your health, cancer stage and cell type.
P/D can’t cure mesothelioma, but it can help control the cancer. It may improve symptoms like chest pain and trouble breathing. Some patients live longer after this surgery. Your doctor will talk with you about your goals and what to expect.
Yes, there are other options besides pleurectomy for mesothelioma. One is a more aggressive surgery called extrapleural pneumonectomy, which removes a lung and nearby tissues. Some patients may also try chemo or immunotherapy instead. Your doctor will help find the safest and most effective plan for you.
In some cases, doctors may repeat a pleurectomy if mesothelioma comes back. It depends on your overall health and how much cancer has spread. Your care team will check if another surgery is safe and helpful.
Stay up-to-date on treatment, research, clinical trials, doctors and survivors
The information on this website is proprietary and protected. It is not a substitute for professional medical advice, diagnosis or treatment. Any unauthorized or illegal use, copying or dissemination will be prosecuted. Please read our privacy policy and terms of service for more information about our website.
This website and its content may be deemed attorney advertising. Prior results do not predict a similar outcome.
The Mesothelioma Center’s claim as the most trusted resource is based on our more than 150 5-star Google and BBB reviews. Our organization also helps more than half of all mesothelioma patients annually diagnosed.
Your web browser is no longer supported by Microsoft. Update your browser for more security, speed and compatibility.
If you are looking for mesothelioma support, please contact our Patient Advocates at (855) 404-4592
The Mesothelioma Center at Asbestos.com has provided patients and their loved ones the most updated and reliable information on mesothelioma and asbestos exposure since 2006.
Our team of Patient Advocates includes a medical doctor, a registered nurse, health services administrators, veterans, VA-accredited Claims Agents, an oncology patient navigator and hospice care expert. Their combined expertise means we help any mesothelioma patient or loved one through every step of their cancer journey.
More than 30 contributors, including mesothelioma doctors, survivors, health care professionals and other experts, have peer-reviewed our website and written unique research-driven articles to ensure you get the highest-quality medical and health information.
My family has only the highest compliment for the assistance and support that we received from The Mesothelioma Center. This is a staff of compassionate and knowledgeable individuals who respect what your family is experiencing and who go the extra mile to make an unfortunate diagnosis less stressful. Information and assistance were provided by The Mesothelioma Center at no cost to our family.LashawnMesothelioma patient’s daughter


Selby, K. (2026, February 18). Pleurectomy/Decortication for Mesothelioma. Asbestos.com. Retrieved March 3, 2026, from https://www.asbestos.com/treatment/surgery/pleurectomy/
Selby, Karen. "Pleurectomy/Decortication for Mesothelioma." Asbestos.com, 18 Feb 2026, https://www.asbestos.com/treatment/surgery/pleurectomy/.
Selby, Karen. "Pleurectomy/Decortication for Mesothelioma." Asbestos.com. Last modified February 18, 2026. https://www.asbestos.com/treatment/surgery/pleurectomy/.

Dr. Andrea Wolf is the Director of the New York Mesothelioma Program at Mount Sinai in New York City. She focuses on multidisciplinary treatment, clinical research, community outreach and education.
Our fact-checking process begins with a thorough review of all sources to ensure they are high quality. Then we cross-check the facts with original medical or scientific reports published by those sources, or we validate the facts with reputable news organizations, medical and scientific experts and other health experts. Each page includes all sources for full transparency.
Please read our editorial guidelines to learn more about our content creation and review process.
