Get answers about treatment, top doctors, and financial support from the nation’s most trusted mesothelioma resource.
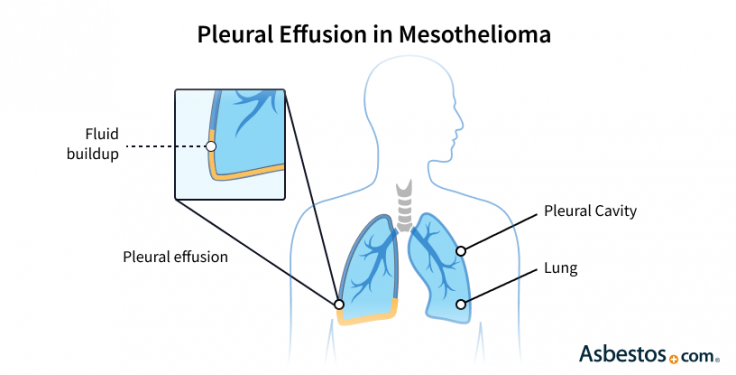
Get Your Free GuidePleural effusion is extra fluid between the lungs and chest wall. Most mesothelioma patients experience this symptom. It can cause chest pain and trouble breathing. Draining the fluid is often one of the first treatments.
Pleural effusion associated with mesothelioma is fluid build up between the chest wall and the lungs, also known as “water on the lungs.” This is a common problem for people with mesothelioma. When fluid collects in the pleural cavity, it can make breathing painful and more difficult.
Key Facts About Pleural Effusion
Pleural effusions often happen early in peoples’ pleural mesothelioma journeys. Dr. Jeffrey Velotta, thoracic surgeon at Kaiser Permanente Oakland Medical Center, tells us, “A pleural effusion is fluid that forms from the pleural lining, secreting usually as a blockage or as a result of mesothelioma in the pleural lining.”
The main types of pleural effusions are grouped based on how the fluid forms. One group includes fluids that collect when pressure changes or low protein levels in the blood cause leaking. These are called transudates. The other group includes fluids that develop when illness or injury inflames or damages the lung lining. These are called exudates.
Sometimes, the fluid also contains blood (hemothorax), lymph fluid (chylothorax) or pus (empyema). Doctors test the fluid to identify its type and cause, so they can choose the best treatment.
Pleural Effusion Types
Some types of pleural effusion are associated with pleural thickening, and some more than others. Effusions involving intense inflammation or cancers like mesothelioma can cause pleural thickening. Malignant pleural effusions often cause inflammation and scarring that lead to this thickening.
Common causes of pleural effusion include irritation from bacteria, viruses and cancer cells like mesothelioma cells. Infections and cancerous cells create irritation in the lining around the lungs. This irritation promotes excess fluid production and collection in the thoracic cavity. As mesothelioma tumors spread over this lining, called the pleura, they can also block lymphatic vessels or blood flow, leading to fluid accumulation.
Causes of Pleural Effusion
When fluid drainage is blocked, excess fluid builds up around the lungs. This happens because the normal balance between fluid production and removal is disrupted. This causes fluid to accumulate faster than it can be cleared. Over time, this buildup can compress the lungs and make it harder to breathe comfortably.
Get answers about treatment, top doctors, and financial support from the nation’s most trusted mesothelioma resource.
Get Your Free GuidePleural effusion isn’t just a hallmark symptom of mesothelioma but also a window into how the tumor disrupts normal lung function. The disease lowers important proteins in the blood, such as albumin, which normally keep fluid inside blood vessels. When these protein levels drop, fluid leaks out and collects around the lungs.
This extra fluid can make breathing harder and cause discomfort. Mesothelioma survivor Michael Bederman tells us he experienced shortness of breath from pleural effusions for a year and had them drained every few months. When he requested a biopsy, doctors confirmed the cause was pleural mesothelioma.
Michael Bederman says, “Everything with me will work out for the best. I don’t sit around feeling sorry for myself. Not at all. I’m grateful for every day and for all the help I’ve received. I look for the good in everything.”
Symptoms of mesothelioma pleural effusion manifest as shortness of breath, cough or chest pain as the increasing fluid constricts the lungs and makes breathing increasingly difficult. Over time, difficulty breathing leads to other symptoms such as fatigue and weight loss.
The more fluid that exists, the more symptoms present themselves, making breathing more challenging. However, a 2025 study in the Journal of Clinical Medicine found that the volume of an effusion didn’t impact survival.
Common Pleural Effusion Symptoms
Consult a doctor if you have any symptoms. Doctors can drain the fluid and provide oxygen and medication for comfort. Without treatment, pleural effusions can become infected or cause lung collapse.
Doctors usually confirm a pleural effusion diagnosis with imaging scans. X-rays, CT scans or ultrasounds will confirm the presence of fluid buildup and show doctors where the effusion is located.
Tools Used to Diagnose Pleural Effusion
To determine the specific type of pleural effusion, pleural fluid is drained with a procedure called thoracentesis. The fluid is then examined. Its contents will confirm if there are atypical or cancer cells present. The sooner doctors diagnose the condition and determine the cause, the sooner they can develop an appropriate treatment plan.
In mesothelioma, pleural effusions house cancerous cells. Specialized procedures called cytology tests look for cancer cells in fluid, aiding in mesothelioma diagnosis. This is particularly important for those with a history of asbestos exposure.
Patient Advocate Snehal Smart, M.D., tells us, “The fluid is drained, and a cytology exam, which is the study of the cells, is performed. Any presence of mesothelial cancer cells would indicate a diagnosis of mesothelioma.”
A 2025 study in Radiology and Oncology reported that the presence of a protein called Fibulin-3 in a pleural effusion could be a strong indicator or biomarker of mesothelioma. The study showed that higher fibulin-3 levels were present in people with advanced or more aggressive disease, but the test didn’t necessarily predict how long they would live.
Treatment for pleural effusion includes draining the fluid for symptom relief and restoring breathing function. Doctors may also recommend surgeries for the prevention of future occurrences. Many people with mesothelioma-related pleural effusions have multiple treatments, especially in later stages.
For example, someone may have a thoracentesis and then a surgical procedure called pleurodesis if the fluid comes back. Each treatment is done based on the cause of the fluid and severity.
Pleural Effusion Treatments
A 2025 report in Pulmonary Therapy discussed how the intrapleural catheter provides a conduit into the pleural space and can be particularly helpful for mesothelioma treatment. Doctors can use it to direct treatment locally to the pleura, where the primary source of cancer often lies.
The outlook for pleural effusion depends on its cause. Because the prognosis for mesothelioma is generally poor, the outlook for effusions linked to this aggressive cancer is also generally poor. Pleural effusions indicate advanced disease and tumor effects disrupting lung function.
If heart or liver failure is the cause, the prognosis relies on your overall health and how available and effective treatments are for you. Early treatment can assist people with symptoms. Even in advanced cases, draining fluid affords comfort and improved respiratory function. Support groups like our Facebook support group, as well as clinical trials can offer hope for better outcomes.
Yes, preventing or treating the underlying cause can help you reduce the risk of pleural effusions. For example, avoiding asbestos exposure as much as possible, treating any infections promptly and managing heart or liver dysfunction can reduce the risk of fluid buildup. Cancer prevention and healthy habits for the heart and lungs, such as a balanced diet, regular exercise and quitting smoking, are also effective ways to prevent pleural effusions.
Life expectancy with pleural effusion depends on the cause and your overall health. For mesothelioma patients, survival time depends on the management of the pleural effusion and the cancer’s progression. Supportive care can improve comfort and quality of life. It includes symptom management and treatments.
Yes, pleural effusion can return after treatment. This is common in chronic conditions like mesothelioma. Some patients may need ongoing treatments, like a catheter for at-home drainage. An indwelling catheter can manage fluid buildup and ease symptoms over time.
The time for pleural effusion to resolve depends on the underlying cause and the associated treatment. Some cases may improve within weeks with treatment. Others, especially mesothelioma-related effusions, may need long-term care.
Preventing pleural effusion in mesothelioma is tough. However, proactive care can reduce symptoms. Chemotherapy might reduce fluid, shrinking tumors. Also, pleurodesis that seals the pleural space can stop extra fluid from building up.
Stay up-to-date on treatment, research, clinical trials, doctors and survivors
The information on this website is proprietary and protected. It is not a substitute for professional medical advice, diagnosis or treatment. Any unauthorized or illegal use, copying or dissemination will be prosecuted. Please read our privacy policy and terms of service for more information about our website.
This website and its content may be deemed attorney advertising. Prior results do not predict a similar outcome.
The Mesothelioma Center’s claim as the most trusted resource is based on our more than 150 5-star Google and BBB reviews. Our organization also helps more than half of all mesothelioma patients annually diagnosed.
Your web browser is no longer supported by Microsoft. Update your browser for more security, speed and compatibility.
If you are looking for mesothelioma support, please contact our Patient Advocates at (855) 404-4592
The Mesothelioma Center at Asbestos.com has provided patients and their loved ones the most updated and reliable information on mesothelioma and asbestos exposure since 2006.
Our team of Patient Advocates includes a medical doctor, a registered nurse, health services administrators, veterans, VA-accredited Claims Agents, an oncology patient navigator and hospice care expert. Their combined expertise means we help any mesothelioma patient or loved one through every step of their cancer journey.
More than 30 contributors, including mesothelioma doctors, survivors, health care professionals and other experts, have peer-reviewed our website and written unique research-driven articles to ensure you get the highest-quality medical and health information.
My family has only the highest compliment for the assistance and support that we received from The Mesothelioma Center. This is a staff of compassionate and knowledgeable individuals who respect what your family is experiencing and who go the extra mile to make an unfortunate diagnosis less stressful. Information and assistance were provided by The Mesothelioma Center at no cost to our family.LashawnMesothelioma patient’s daughter


Asbestos.com. (2026, February 13). Pleural Effusion and Mesothelioma. Retrieved March 5, 2026, from https://www.asbestos.com/mesothelioma/pleural-effusion/
"Pleural Effusion and Mesothelioma." Asbestos.com, 13 Feb 2026, https://www.asbestos.com/mesothelioma/pleural-effusion/.
Asbestos.com. "Pleural Effusion and Mesothelioma." Last modified February 13, 2026. https://www.asbestos.com/mesothelioma/pleural-effusion/.

Dr. Chelsea Alvarado earned her doctorate from the University of Maryland School of Medicine in Baltimore, Maryland. She received a Bachelor’s degree in biochemistry from Temple University in Philadelphia. She currently works as a freelance medical writer and is passionate about making medical science accessible to all.
Our fact-checking process begins with a thorough review of all sources to ensure they are high quality. Then we cross-check the facts with original medical or scientific reports published by those sources, or we validate the facts with reputable news organizations, medical and scientific experts and other health experts. Each page includes all sources for full transparency.
Please read our editorial guidelines to learn more about our content creation and review process.
