Jim McWhorter was told an injury-prompted X-ray was clear, but pleural thickening was noted in his record. A later surgery found tumors. It turns out that the pleural thickening led to his pleural mesothelioma diagnosis.
Pleural Thickening and Asbestos
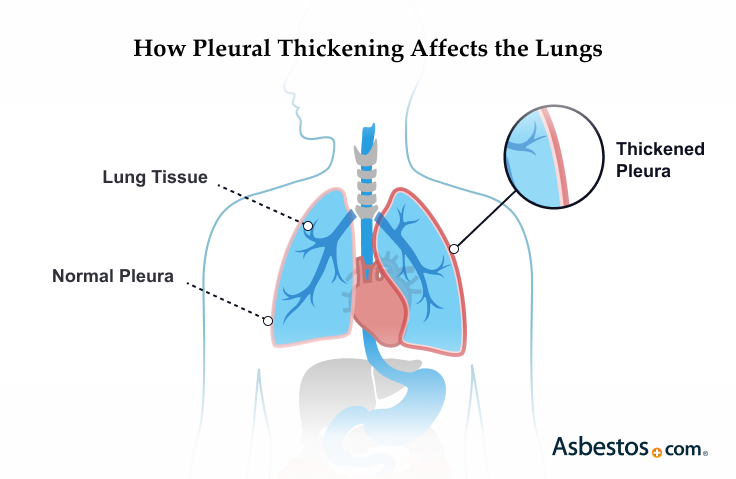
Pleural thickening means scar tissue has built up on the lining of the lungs. This can happen after asbestos exposure, injury or infection. It isn't cancer, but may be an early sign of mesothelioma. Treatment can't cure it, but can ease symptoms and help you feel better.
Pleural Thickening and Mesothelioma
Pleural thickening isn’t cancer, but it may be an early sign of it. Asbestos can cause both pleural thickening and mesothelioma. If you have pleural thickening, see your doctor often. In some people, it gets worse and leads to more serious illness.
Key Facts About Pleural Thickening
- About 50% of asbestos-exposed workers develop pleural thickening.
- More than 90% of mesothelioma patients experience pleural thickening.
- Pleural thickening can significantly increase the risk of pleural mesothelioma.
Recent studies show finding pleural thickening early can lead to better care. Registered Nurse Sean Marchese says, “It can help find mesothelioma sooner. This means more ways to treat it and feel better.”
Types of Pleural Thickening
In pleural mesothelioma, pleural thickening is usually diffuse or focal. These terms describe how much of the lining is affected. The thickening can be noncancerous, cancerous or another type.
Each type affects the lungs differently. That changes how doctors treat it and what to expect.
Main Types of Pleural Thickening
- Diffuse pleural thickening: Scarring spreads across a large part of the lung lining. It often happens after heavy asbestos exposure.
- Focal pleural thickening: Scarring stays in one area. It’s usually milder than diffuse thickening.
Knowing what caused the thickening helps doctors plan care. They keep a close eye on both types to protect your lungs and catch signs of cancer early.
Diffuse Pleural Thickening
Diffuse pleural thickening means a large area of the lungs’ lining has scarring. This can make it harder to breathe. This type is strongly linked to heavy asbestos exposure.
Diffuse Pleural Thickening Types
- Benign pleural thickening: This type isn’t cancer. It happens when thick, fibrous tissue builds up in the lung lining.
- Malignant pleural thickening: This kind covers 50% or more of one pleura or 25% of both pleurae. It can be a sign of pleural mesothelioma.
Doctors recommend people with diffuse thickening regularly track their lung health. Without care, this condition could lead to pleural mesothelioma.
Focal Pleural Thickening
Focal pleural thickening means scarring in one small area of the lungs’ lining. It can happen after minor asbestos exposure or past infections. While it’s usually less serious, doctors still need to watch it closely.
Focal Pleural Thickening Types
- Apical pleural thickening: Scarring at the top of one lung.
- Biapical pleural thickening: Also called bilateral apical. Scarring at the top of the pleura and both lungs.
- Nodular pleural thickening: Scarring that forms small lumps or nodules.
Imaging scans can help find this condition early. Early care may lower the risk of more serious lung problems like mesothelioma.

Get a free guide with the latest mesothelioma treatments and clinical trials.
Get Yours NowWhat Causes Pleural Thickening?
The main cause of pleural thickening is breathing in asbestos. Other causes include infections or chest injuries. Asbestos dust has tiny fibers that can get stuck in the lining of the lungs. Over time, these fibers cause irritation and scarring. This scar tissue can build up and lead to pleural thickening.
Causes of Pleural Thickening
Discuss your risk for pleural thickening with your doctor. If you have a history of asbestos exposure, ask about regular screenings.
A classic study in the Journal of Occupational Medicine and Toxicology looked at asbestos. Some workers were found to have pleural thickening after exposure to the mineral. It developed in 5% to 13.5% of workers, often 3 to 34 years after their first exposure.
What Are the Symptoms of Pleural Thickening?
The most common symptoms of pleural thickening are breathlessness, chest pain and coughing. Symptoms usually develop slowly and can be hard to notice at first. Catching these signs early can lead to better care and outcomes.
Common Pleural Thickening Symptoms
- Breathlessness
- Chest pain
- Coughing
- Fatigue
- Fever
- Pain when inhaling or exhaling
- Shortness of breath (dyspnea)
Anyone with lasting breathing problems or chest discomfort should talk to a doctor. Regular screenings are crucial for preventing asbestos-related diseases. This is especially critical for those with known asbestos exposure.
How Doctors Diagnose Pleural Thickening

Doctors use X-rays, CT scans and MRIs to look for pleural thickening. Finding it early can help guide better treatment and improve outcomes.
They also run tests to rule out other conditions like pleural plaques. These are small, flat spots on the outside of the lungs. Unlike plaques, pleural thickening is widespread scarring that can make the lungs stiff. Doctors also check for signs of asbestos cancers, like pleural mesothelioma.
Telling your doctor about any asbestos exposure helps with a clear diagnosis. If you’re unsure about your diagnosis, getting a second opinion is always an option.
Biopsy
A biopsy removes a small piece of tissue from the lining of the lungs. Doctors look at it under a microscope to find out what’s causing the thickening.
Your doctor may use a needle or a small camera (thoracoscopy) depending on where the thickening is. The results help confirm a diagnosis and guide the best treatment plan for you. Recent research suggests CT-guided biopsies are also a safe and effective option for collecting pleural tissue.
Imaging Scans
Doctors use the same imaging scans for pleural thickening and mesothelioma. On chest X-rays, pleural thickening shows as a thick white line along the lung’s edge. PET scans and MRIs help tell pleural thickening apart from mesothelioma.
CT scans provide detailed images showing the extent of thickening. These scans help catch problems early so treatment can start sooner.
Pam McWhorter shares with us how imaging scans that found pleural thickening eventually led to her husband’s pleural mesothelioma diagnosis. She tells us that after an X-ray, “They noted on his medical records that there was thickening on the outside of the left lung.” Then he had a CT scan. Pam tells us the CT scan report said, “‘Nodular thickening, suspect for mesothelioma, doctors should take immediate action.’”
Pleural Thickening Treatment
There is no cure for pleural thickening. But supportive treatment can help manage it. The best options are to quit smoking, stay active and do rehab.
Treatments That Ease Pleural Thickening
- Complementary therapies: Relaxation techniques and meditation may ease symptoms such as pain.
- Exercise: Respiratory exercises can improve cardiorespiratory functions.
- Medications: Doctors may use steroids to ease breathlessness.
- Oxygen therapy: Using inhalers may help less severe cases.
- Pulmonary rehabilitation: People perform breathing techniques and exercises over 2-3 weeks.
- Smoking cessation: Lung function may improve when patients stop smoking.
Surgery, such as pleurectomy, may help severe cases of pleural thickening. People with severe breathing issues may use portable oxygen tanks.
Doctors Who Treat Pleural Thickening
Pulmonologists and pleural specialists have the expertise to diagnose and treat pleural thickening. They can recommend follow-up care and watch your condition for signs of progression.
Our Patient Advocates can match you with a top specialist near you. Our team has been helping people find doctors since 2006.

Maywood, Illinois
Pleural Specialist | Thoracic Surgery
Expertise: Thoracic Surgery Mesothelioma Lung and Lung/Heart Transplantations Pleurectomy and Decortication Robotic Surgery
Languages: English, Tamil

Oakland, California
Pleural Specialist | Thoracic Surgery
Expertise: Pleural Mesothelioma, Lung Cancer, Cardiothoracic Surgery, Cardiac Surgery and Surgical Oncology
Languages: English

New York, New York
Pleural Specialist | Thoracic Surgery
Expertise: Pleural Mesothelioma, Pleurectomy and Decortication Surgery, Lung Cancer, VATS, Lobectomy, Thoracotomy and Clinical Research
Languages: English, Spanish

Tampa, Florida
Pleural Specialist | Thoracic Surgery
Expertise: Pleural Mesothelioma, Lung Cancer, Thoracic Diseases, Minimally Invasive Surgery, Pleurectomy and Decortication Surgery
Languages: English, Spanish, French, Arabic
If you need assistance finding a pleural specialist, our Patient Advocates at The Mesothelioma Center can match you with a top doctor near you. Our team of Patient Advocates has been helping patients find doctors since 2006.
Common Questions About Pleural Thickening
- Can smoking cause pleural thickening?
-
Asbestos is the primary cause of pleural thickening. Some data indicates a correlation between smoking and the progression of pleural thickening. Smoking limits lung function. It’s also proven to be a cause of other respiratory diseases, such as lung cancer.
- Can pleural thickening affect your lifespan?
-
In most cases, pleural thickening won’t affect lifespan. But this condition may be a sign of more serious underlying conditions. These include malignant pleural mesothelioma or other cancer. Your doctor will determine how serious your pleural thickening is with diagnostic tests.
- Have there been any asbestos lawsuits related to pleural thickening?
-
Yes, Miller v. Armstrong World Industries, Inc. in 1991 was a precedent-setting court case. Raymond Miller was an insulator who worked with asbestos products. He eventually developed pleural thickening. There is now an asbestos trust fund, the Armstrong World Industries Asbestos Trust. It accepts claims from people who were exposed to the company’s asbestos products. and became ill.
- Is pleural thickening serious?
-
Pleural thickening is not always a serious condition. But if it’s left untreated, it can advance into other, more dangerous stages such as encasement of the lung. This condition causes restrictive lung disease. Pleural thickening is also a sign of significant asbestos exposure. Pleural mesothelioma’s main cause is asbestos exposure.
- What is the difference between benign and malignant pleural thickening?
-
Benign pleural thickening means cancer tumors did not lead to the thickened tissue. Fibrous tissue that builds on top of itself is the cause. Pleural mesothelioma or cancer that spreads from another location causes malignant pleural thickening




