Pleural Effusion and Mesothelioma
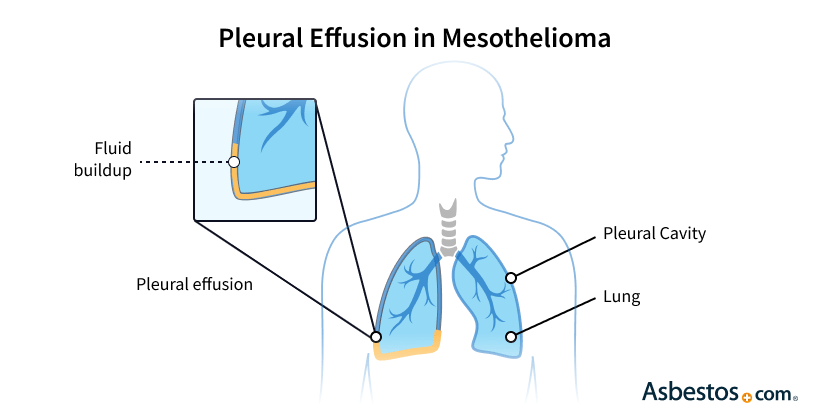
Pleural effusion occurs when fluid builds up between the chest wall and the lungs. This is a common symptom of pleural mesothelioma. Side effects of pleural effusion include shortness of breath (dyspnea), chest pain and discomfort.
What Is Pleural Effusion?
Pleural effusion is when fluid builds up between the chest wall and the lungs, also known as “water on the lungs.” This is a common problem for people with mesothelioma. When fluid collects in the pleural cavity, it can make it hard and painful to breathe.
Normally, a small amount of fluid helps the lungs move smoothly. But when there is too much fluid, it can cause pressure on the lungs. This makes it hard to breathe and can hurt the chest.
“A pleural effusion is fluid that forms from the pleural lining, secreting usually as a blockage or as a result of mesothelioma in the pleural lining,” said Dr. Jeffrey Velotta, thoracic surgeon at Kaiser Permanente Oakland Medical Center. “Because the fluid compresses onto the chest wall, patients often present with severe chest pain.”
Pleural effusion often shows up early in mesothelioma patients. It happens when the cancer affects the thin membranes around the lungs. This causes too much fluid to build up.
For mesothelioma patients, managing pleural effusion is important. It can help improve breathing and quality of life. Knowing the causes, symptoms and treatments of pleural effusion can help patients and their caregivers.
- Chest X-rays, CT scans and thoracentesis are used to diagnose pleural effusions and determine if they are related to cancer.
- Managing pleural effusion through procedures like thoracentesis or pleurodesis can help improve breathing and overall quality of life.
- Mesothelioma tumors can block lymphatic vessels or blood flow in the pleura, leading to fluid accumulation.
- Pleural effusion is common in mesothelioma, with up to 90% of patients experiencing it, often as an early sign of the disease.
- Symptoms include shortness of breath, chest pain, dry cough and fatigue, which worsen with larger fluid volumes.
Mesothelioma & Pleural Effusion
Most patients with pleural mesothelioma, about 90%, have pleural effusion during their illness. It can often be one of the first signs of mesothelioma. The pleural cavity has a small amount of fluid to help with breathing. This fluid is made and removed by the body. When this balance is upset, because of sickness or cancer, fluid builds up and causes pleural effusion.
Cancer cells can block the lymphatic vessels. They help remove excess fluid. When these vessels are blocked, fluid starts to build up. In mesothelioma patients, a protein called albumin is often low. Albumin helps keep fluids in blood vessels. When levels are low, fluid can leak into the pleura, adding to pleural effusion. Tumors can also make blood vessels leak. This causes more fluid to enter the pleural cavity and adds pressure to the lungs.
A 2023 observational study from Kyuongpook National University and Ajou University Medical Center noted that non-expandable lung is more prevalent in mesothelioma patients, and up to 90% of people with pleural mesothelioma experience pleural effusion.
Types of Pleural Effusion
Some pleural effusions, such as those caused by pleural mesothelioma, may be mild and can disappear. But others linked to mesothelioma may need medical help to avoid serious problems like a lung collapse.
- Exudative Pleural Effusion: This type happens because of infections or cancers like mesothelioma. It has high levels of proteins and cancer cells, making it useful for diagnosis.
- Malignant pleural effusion: This type is often found in cancer patients, like those with pleural mesothelioma.
- Non-malignant pleural effusion: This can happen from infections or heart problems.
- Transudative Pleural Effusion: This type comes from issues not affecting the pleura, like heart failure. The fluid is usually clear and has fewer proteins.
Pleural effusion is different from pulmonary edema. Pulmonary edema is when fluid builds up inside the lungs instead of around them. Both can cause shortness of breath, but they have different causes and treatments.
“After reading the guide, I felt more confident about what was ahead.” – Carla F., mesothelioma survivor
Get Your Free GuideWhat Causes Pleural Effusion?
Pleural effusion can be caused by various diseases, including cancers, infections and inflammatory conditions. When cancer causes a pleural effusion, it’s called a malignant effusion. Both mesothelioma and lung cancer commonly cause malignant effusions.
Even people without a mesothelioma cancer diagnosis but who have been exposed to asbestos are at an increased risk of developing pleural effusions. Pleural effusions can signal a developing asbestos-related disease, such as pleural thickening, and contribute to its progression.
- Alcoholism
- Asbestos exposure
- Blood clot in the lung (pulmonary embolism)
- Heart failure
- High blood pressure
- Liver scarring (cirrhosis)
- Pneumonia
- Smoking
- Surgery
If you have a pleural effusion, your doctor must obtain a fluid sample to determine the cause and the best treatment. Knowing the type of pleural effusion helps doctors find the right treatment. They can test pleural fluid to learn more about the cause.
- Breast and Ovarian Cancer: These cancers can spread to the pleura, causing problems.
- Lung Cancer: This cancer can also lead to pleural effusion.
- Mesothelioma: This is the most common cancer that causes pleural effusion.
Pleural mesothelioma tumors make substances that increase leaks in blood vessels. These leaks allow blood, lymphatic fluid and water to leave the blood system and enter the pleural cavity. These fluids build up, causing exudative pleural effusion.
What Are the Symptoms of Pleural Effusions?
The most common symptoms of pleural effusion in pleural mesothelioma patients are fatigue, shortness of breath and chest pain. These symptoms depend on the amount of fluid present. Some small pleural effusions may not cause symptoms, but larger ones can lead to big problems.
- Chest Pain: This pain can be sharp and worse when breathing deeply.
- Difficulty Breathing When Lying Down: The extra weight from fluid can make lying down uncomfortable.
- Dry Cough: Fluid can irritate the lungs and cause a dry cough.
- Fatigue: Not getting enough air can make a person feel tired.
- Shortness of Breath: Fluid buildup can make it hard to breathe deeply.
Although pleural effusions can resolve by itself, consult a doctor if you have any symptoms. Without treatment, pleural effusions can become infected or cause lung collapse.
How Do Doctors Diagnose Pleural Effusions?
Doctors use different methods, including X-rays or CT scans, to diagnose pleural effusion. These tests detect fluid buildup and help determine if the underlying cause is mesothelioma or another condition.
- Chest X-ray: This test shows if there is fluid. Pleural effusions often appear as cloudy spots on an X-ray.
- CT Scan: This test gives a clearer picture of the pleural cavity. It helps doctors see how big the effusion is and what might be causing it.
- Thoracentesis: A doctor uses a needle to take fluid out for testing. This can help find cancer cells and help with diagnosis.
A chest X-ray or thoracentesis is the best way to determine the cause. Thoracentesis involves ultrasound-guided fluid removal from the pleural cavity using a needle.
The Importance of Diagnosing Mesothelioma for Mesothelioma Patients
Diagnosing mesothelioma from a pleural effusion is vital to an early diagnosis. Doctors test this fluid for cancer cells. Patient Advocate Snehal Smart, M.D. at The Mesothelioma Center, explains, “That fluid is drained, and a cytology exam, which is the study of the cells, is performed. Any presence of mesothelial cancer cells would indicate a diagnosis of mesothelioma.”
If fluid testing results suggest mesothelioma, a doctor will order a biopsy. Survivor Michael Bederman experienced shortness of breath from pleural effusions for a year. When he requested a biopsy, doctors confirmed the cause was pleural mesothelioma.
How to Treat Pleural Effusions?
Pleural effusion is commonly treated by catheter placement, thoracentesis and pleurodesis, which are frequently used in mesothelioma care. These procedures remove the fluid and can temporarily improve symptoms.
- Catheter Placement: A catheter can drain fluid regularly at home.
- Pleurectomy/Pleural Decortication: This surgery removes tumors and the pleura. It helps the lungs expand better.
- Thoracentesis: This method helps by removing fluid temporarily.
Each treatment can help improve breathing and reduce symptoms. Treating the cause of the pleural effusions, such as with cancer therapy, can prevent them from coming back.
What Is the Prognosis for Pleural Effusion?
The prognosis or outlook for pleural effusion depends on the cause. While the prognosis is generally poor for people with malignant pleural effusion, it can vary significantly for each individual patient.
People with pleural mesothelioma and pleural effusion tend to live a bit longer than people with lung cancer, living an average of almost a year compared to 2-3 months. Treating mesothelioma can extend people’s lives an average of two years, with some living even longer.
Research in new and emerging therapies is ongoing to improve prognosis for malignant pleural effusion patients. For people with cancer-related pleural effusions, joining a support group can help survivors cope with the stress related to their diagnosis and prognosis. The Mesothelioma Center, for example, offers a private Facebook support group exclusively for mesothelioma patients, their families and caregivers.
Common Questions About Pleural Effusions
- How long can you live with pleural effusion?
-
Life expectancy with pleural effusion varies. It depends on the cause and the person’s health. For mesothelioma patients, survival time depends on two factors. One is the management of the pleural effusion. The other is the cancer’s progression. Supportive care can improve comfort and quality of life. It includes symptom management and treatments.
- Can pleural effusion come back after treatment?
-
Yes, pleural effusion can return after treatment. This is common in chronic conditions like mesothelioma. Some patients may need ongoing treatments, like a catheter for at-home drainage. It can manage fluid buildup and ease symptoms over time.
- How long does it take for pleural effusion to resolve?
-
The time for pleural effusion to resolve varies widely. It depends on the cause and the treatment. Some cases may improve within weeks with treatment. Others, especially cancer-related effusions, may need long-term care.
- Can pleural effusion be prevented in mesothelioma patients?
-
Preventing pleural effusion in mesothelioma is tough. However, proactive care can reduce symptoms. Chemotherapy might cut down fluid by shrinking tumors. Also, pleurodesis can stop extra fluid by sealing the pleural space.





