Karen R. was diagnosed with pleural mesothelioma after deciding to receive an optional scan that wasn’t covered by her insurance during an annual check-up. “The doctors detected fluid around my lungs during this scan. If I had not chosen to get this optional scan the cancer would have gone undetected for much longer,” Karen said.
Mesothelioma Imaging Scans
Mesothelioma imaging scans include X-rays, CT scans, MRIs and PET scans. They're a key part of diagnosing this rare cancer. Imaging scans for mesothelioma let doctors see if the cancer has spread.
Role of Imaging Scans in Mesothelioma Diagnosis
Mesothelioma imaging scans are an important part of a diagnosis. Doctors may arrange regular scans for those with a history of asbestos exposure. These screenings can find early signs of disease. Scans may show scarring, fluid, thickening and tumors. This can lead to an earlier diagnosis.
Your scans are helpful when seeking a second opinion. Dr. Jeffrey Velotta is a thoracic surgeon at Kaiser Permanente Oakland Medical Center. He tells us, “For consultations or second opinions, really it’s about the imaging. What we really need to see first is the CT and PET scans.” A mesothelioma expert can look at all of your previous images and tests.
- More than 607 million imaging scans were taken in the U.S. in 2023.
- Doctors use imaging scans with a biopsy to confirm a mesothelioma diagnosis.
- Doctors use scans to check the spread of tumors. This is known as mesothelioma staging.
In addition to using imaging for diagnosis, it’s used to stage mesothelioma. Doctors often base mesothelioma treatment plans on how far tumors have spread. Stage 1 and 2 patients generally have more options than stage 4 patients.
Mesothelioma tumors can be hard to see on some scans. Tumors can appear hazy on X-rays, for example. Biopsy is necessary to confirm a diagnosis. Yet, new technology is growing imaging’s role in diagnosis. The International Mesothelioma Interest Group held a conference. It focused on imaging scans for mesothelioma. They report a growing role for imaging in assessing and managing patients.
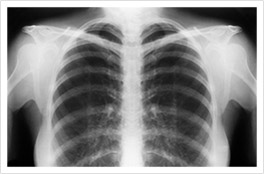
X-Rays Scans
Doctors usually use X-rays as the first imaging test to check for mesothelioma. X-rays only provide a 2D view. There are limits to their usefulness in mesothelioma diagnosis. But they can identify abnormalities. For example, an X-ray can show fluid buildup or tumors.
In a mesothelioma X-ray, pleural tumors can appear as wispy white areas. Tumors can also distort the normal shape of the lungs and, in some cases, elevate the diaphragm. These changes are easily visible in an X-ray.
- X-ray scans use a small amount of radiation.
- This radiation produces a 2D image showing the inside of the body.
- The use of X-rays is safe.
- They expose you to the same level of radiation you naturally encounter in the course of 10 days.
Michael Cole, a survivor of pleural mesothelioma, shares his X-ray story with us. A cough and lack of energy sent him to his doctor. Michael says, “They listened to my chest, took an X-ray and told me to go straight to the hospital. They quickly drained 2 liters of foul-looking fluid out of my right lung.” He was diagnosed with mesothelioma 4 days later.
Abnormalities on an X-ray can point doctors toward a diagnosis. These scans are a key first step in finding mesothelioma. They’re safe and widely available. This makes X-rays a useful tool for diagnosing lung diseases.
Find the top cancer centers trusted by mesothelioma patients nationwide.
Get Help NowCT Scans (Computed Tomography)
CT scans provide detailed cross-sectional images. These images allow doctors to visualize abnormalities. CT scans for mesothelioma can be limited to the chest or abdomen. They can also scan the entire body.
CT scans are perhaps the most important scan used to detect mesothelioma. A 2023 study in the Japanese Journal of Radiology says, “CT scans are paramount for primary staging and treatment planning.” They can help diagnose and stage mesothelioma. They can also help with surgical planning. Recent research has shown CT scans may even be able to identify mesothelioma cell types.
- A CT scanner takes hundreds of small X-rays.
- A computer uses the X-ray data to create “slices,” or cross-sectional images.
- The machine rotates around your body and moves you through it.
Images from a CT scan will look different depending on the type of mesothelioma you have. If you have pleural mesothelioma, a CT scan may show abnormal thickening of the pleura. If you have peritoneal mesothelioma, the scan may show tumors on the peritoneum.
Joey Barna is a pleural mesothelioma survivor. He spoke with us about his mesothelioma imaging scans. He shares, “I went to the hospital, and they thought I had pneumonia because they saw fluid on my lung. A week later I had a follow-up X-ray, and they saw that the fluid was still there. My primary doctor sent me for a CT scan. Fluid had built up and was pressing against my lung. It was preventing me from breathing properly.”
PET Scans (Positron Emission Tomography)
PET scans are helpful in diagnosing mesothelioma. They can find even the smallest of tumors. These scans can help identify areas where cancer has spread as well. This makes PET scans very useful for both early detection and staging of mesothelioma.
PET scans are often combined with CT scans to form PET/CT scans. Together, the scans provide a complete view. This type of imaging combines PET’s metabolic detection with CT’s detailed anatomy.
- PET scans use radioactive isotopes combined with sugar (glucose).
- A radioactive tracer is given via an IV.
- This tracer acts like a tiny glowing marker.
- It helps doctors spot areas in your body with high metabolic activity.
- Seeing the “glow” helps spot mesothelioma cells.
These scans can assess tumors’ sizes and locations. This provides vital information for treatment planning. Research suggests PET/CT scans may be better than CT and MRI for staging mesothelioma. They give key insights into the disease’s progression and outlook.
PET scans are also key for tracking treatment response. Doctors can compare PET scans over time. They show if cancer is responding to therapy, stable or progressing. It’s crucial for adjusting treatment. PET are expensive and there’s limited availability. However, scans remain a vital tool in managing mesothelioma.
MRI Scans (Magnetic Resonance Imaging)
MRI scans provide detailed images of soft tissues. These images are key for detecting, diagnosing and staging mesothelioma. MRI is good at identifying changes in soft tissue. MRIs can show how much a tumor has invaded nearby tissues and organs. This information is vital for staging the disease.
Newer MRI techniques have improved mesothelioma detection. They highlight small changes the magnetic field causes at the atomic level. These advanced imaging techniques provide additional detail. MRIs are invaluable for a complete assessment of the disease.
- MRIs use powerful magnetic fields and radio waves.
- The MRI machine makes a strong magnetic field around you.
- Radiofrequencies pulse through your body.
- Mesothelioma tumors respond differently than healthy tissue.
- Contrast dye is often used to highlight any tumors or other abnormalities.
Kasie Coleman tells us about her MRI. She began having symptoms in October 2008. She shares, “I was on a quest to find out what was going on with my ailing body. After multiple tests, my doctor sent me for an MRI. Two hours after my test, I received a call. I drove back to the office and was told multiple tumors were found.”
Her MRI was in May 2009. She didn’t get her diagnosis of peritoneal mesothelioma until July 2010. This underscores the value of a second opinion with a mesothelioma specialist. You can have all your scans sent to a doctor who has mesothelioma experience to review.
Comparing Mesothelioma Imaging Scans: Which Is Best?
CT and PET scans, MRIs and X-rays are all important part of diagnosis and staging. They can all help detect mesothelioma and assess its spread. But MRIs have advantages over other imaging scans for mesothelioma. Their detailed images help find tumors earlier than X-rays or CT scans.
Unlike X-rays and CT scans, MRIs don’t use radiation. So, multiple MRIs are generally considered safe. This makes MRIs a safer option for repeated imaging. This is very helpful for those who need long-term monitoring.
While CT scans aren’t as detailed as MRIs, their images are 3D whereas X-rays are 2D. CT scans provide much more detail than a standard X-ray. They allow doctors to see small tumors throughout the body.
CT scans, however, expose you to about 70 times more radiation than X-rays do. It’s safe to have repeated chest X-rays. Doctors don’t usually do multiple CT scans to avoid the higher radiation.
Monitoring Mesothelioma Treatment with Imaging Scans
People with mesothelioma often have many scans done. Images are taken during diagnosis and staging. These images help to decide the right treatment for that person. It’s also important to do imaging scans for mesothelioma after treatment. They can help track remission and recurrence.
Survivor Tamron Little shares her scan experiences with us. She says, “The frequency of scans can depend on the patient and their progression. Before I had HIPEC surgery, I had a lot of preliminary scans.”
She adds, “After my surgery I had a follow-up CT scan a couple of weeks later. Then, after my doctor saw I was doing well with no cancer being found, it was one every 6 months. Then it was every 18 months up until the 5-year mark.”
Kevin Hession, a pleural survivor, says scans can pick up surgery’s effects. He tells us, “There is a lot of scar tissue around my left lung where they did a lot of work. Looking at it from the CT scans, you can see the scar tissue and it kind of surrounds the left lung.”
What to Expect During a Mesothelioma Scan
When you arrive for your mesothelioma scan, the technologists will guide you. They’ll explain the process and answer your questions. It can also help to talk with your doctor beforehand. They can help prepare you for what to expect in advance.
There are similarities in the process for each imaging type. You’ll need to lie flat on your back for most mesothelioma imaging. X-rays may involve standing or other positions. Staying very still is crucial for clear imaging. If you have limited mobility or pain, let the imaging team know. They can help ensure your comfort.
Mesothelioma Imaging Scan Processes
- Communication: CT and PET techs will talk to you via a speaker. For an MRI, headphones cancel noise and allow communication. Techs may tell you to hold your breath briefly.
- Contrast dye: For CTs and MRIs you may be given a contrast dye orally or intravenously. This enhances image visibility.
- Duration: A CT scan typically only takes about 10 minutes. PET scans and MRIs can take 30 to 90 minutes.
- Radioactive tracer: For PET scans, you’ll have an IV infusion of a radioactive tracer an hour before your scan.
- Results: MRI, CT scan or PET scan results are usually available within a couple of days. A radiologist will write a report your doctor will discuss with you.
An MRI scan is similar to a CT, an MRI is loud. Metal coils in the scanner make booming and banging noises. People wear headphones throughout the scan. Also, the MRI scanner is more enclosed, which can cause anxiety. You will have a distress button to press if you need to stop the scan.
Before an MRI, tell your doctor and the technicians if you have any metal in your body. This includes surgical implants, pacemakers or shrapnel. An MRI’s strong magnetic field can affect metal objects. This could cause serious complications.
Common Questions About Mesothelioma Imaging Scans
- Does asbestos show up on a CT scan?
-
No, asbestos fibers are microscopic. They aren’t visible on imaging scans. A high-powered microscope can see asbestos fibers in a biopsy. The presence of these fibers can help confirm a diagnosis of an asbestos-related disease.
- What are the risks or side effects of mesothelioma imaging scans?
-
X-rays and CT scans use radiation. The exposure from X-rays is considered minimal and safe. CT scans involve significantly more radiation. Repeat CTs are avoided for this reason.
People who receive contrast dye during a CT or MRI may have an allergic reaction. Some people also experience nausea.
Though rare, some people can be allergic to the radioactive tracer in a PET scan. It also involves exposure to radiation. These scans aren’t usually recommended for those who are pregnant.
An MRI might cause temporary effects from the magnetic field. These include dizziness, nausea, a metallic taste or brief flashes of light.
- Can ultrasound detect mesothelioma?
-
Ultrasound can be part of a mesothelioma diagnosis. But its use isn’t common. Soundwaves create its images. These soundwaves don’t travel well through air. So, it is hard to get good images in the chest cavity and abdomen.
While ultrasound’s images aren’t as detailed as CT scans or MRIs, they can be used to look at fluid buildup. Echocardiogram, for example, is a type of ultrasound. Doctors may use it if there’s fluid around the heart. This can help indicate an issue such as pericardial mesothelioma.