Get answers about treatment, top doctors, and clinical trials from the nation’s most trusted mesothelioma resource.
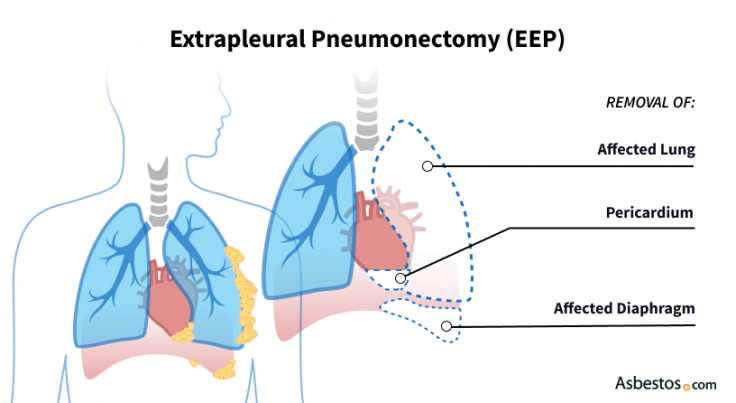
Get Your Free GuideExtrapleural pneumonectomy (EPP) is a type of surgery used for treating pleural mesothelioma. During an EPP, doctors remove the lining of the lung (pleura), the lung, the sack around the heart (pericardium) and the diaphragm. Recovery takes at least 6 to 8 weeks.
An extrapleural pneumonectomy is a surgical procedure for pleural mesothelioma that removes the entire cancerous lung. An EPP can improve your breathing and quality of life. After recovery, people often feel more at ease. This can allow you to return to you daily activities or even resume work.
This mesothelioma procedure gets its name from the original surgery known as a pneumonectomy, which removes only the affected lung. The “extrapleural” means the surgeon goes beyond the entire removal of your lung to include the removal of its pleural lining, nearby lymph nodes and parts of the heart lining and diaphragm.
Key Facts About Extrapleural Pneumonectomy
Dr. Sameer Jhavar, a radiation oncologist at Baylor Scott & White Medical Center, believes an EPP can help certain patients. Dr. Jhavar says, “It all depends on the patient selection. In the right patient population, [EPP] can be done safely and effectively and provide survival hope.”
You may be eligible for EPP for mesothelioma if your doctor believes you can recover from possible complications. You should also be in good overall health. Eligibility is limited if you have the sarcomatoid cell type, late-stage cancer or certain preexisting conditions. Talk with a mesothelioma surgeon to determine if EPP could benefit you.
EPP Eligibility Criteria
Mesothelioma patients with the epithelioid cell type typically have a more favorable response to aggressive surgery because these cells spread more slowly and stick together more readily. In contrast, the sarcomatoid cell type is less likely to benefit from EPP because of its rapid spread and poor prognosis. For biphasic mesothelioma tumors (which contain both epithelioid and sarcomatoid cells), eligibility often depends on the proportion of epithelioid cells present.
The National Comprehensive Cancer Network doesn’t recommend surgery for those whose pleural mesothelioma has progressed beyond stage 3A. Unfortunately, many people are diagnosed after their cancer has progressed to stages 3B or 4.
Surgeons may recommend pleurectomy/decortication for certain people who can’t tolerate the more aggressive EPP surgery. A P/D may be better for people with symptoms like entrapped lung syndrome (one lung is unable to expand fully) and recurrent pleural effusions (extra fluid between the lungs and chest wall).
Before performing EPP, your mesothelioma doctors will test your lung function to ensure your remaining lung will be strong enough to work well on its own. Your doctor will also check your heart health.
EPP Procedure Steps
During an EPP, the anesthesiology team plays a critical role in managing the single remaining lung. They use a special tube to keep the target lung deflated while the other lung continues to function. From the moment surgery begins, the anesthesiologist closely monitors oxygen levels, uses gentle ventilation settings to protect the remaining lung, manages shifts in chest structure and fluid levels, and stands ready to act if oxygen levels drop or blood pressure falls.
Imaging scans let your surgeon see how far the cancer has spread to guide surgical decisions. A PET/CT scan can assess if tumors have spread to the other side of your chest or into your abdomen. An MRI can identify tumors in your chest wall and diaphragm.
Get answers about treatment, top doctors, and clinical trials from the nation’s most trusted mesothelioma resource.
Get Your Free GuideAn extrapleural pneumonectomy can extend survival, reduce symptoms and improve your quality of life. While there is currently no cure for mesothelioma, EPP can help control it. Many people feel better after surgery, with extended survival, and some live for many years.
Benefits of Extrapleural Pneumonectomy
Pleural mesothelioma survivor Michael Cole sought medical advice from mesothelioma pioneer Dr. David Sugarbaker, who worked at Baylor College of Medicine in Houston, in 2015. Sugarbaker recommended an aggressive treatment with EPP and chemo.
“As it has turned out, the EPP with HITHOC followed by four rounds of chemotherapy was not the end of my treatment journey, but rather only the beginning,” Cole tells us. “I believe the aggressive treatment I had in the beginning was absolutely necessary to give me a chance to be here now, and I am grateful for the decision we made.”
Some mesothelioma surgeons believe the lung-sparing pleurectomy and decortication is a safer alternative to EPP. In fact, most surgeons avoid this aggressive procedure. A P/D is ideal for stage 1 pleural mesothelioma, while an EPP can remove visible tumors in patients with stages 2 through 3A. Some surgeons can offer P/D surgery and convert the procedure into an EPP if they discover more cancer than imaging detected.
EPP can offer hope, but the most serious risk is death after surgery. The mortality rate for EPP is higher compared to the less invasive P/D procedure. A 2024 review comparing mortality found a death rate of 6% for EPP and 2.2% for P/D.
Complications can arise after EPP surgery. The 2024 review reported the complication rate ranged between 38% and 68% for EPP. The P/D complication rate ranged between 26% and 58%. Notably, nearly 10% of EPP patients required an unexpected return to the operating room, compared to just 1.5% for P/D patients.
Additionally, according to a 2012 study on multimodal therapy for mesothelioma, local recurrence (cancer returning at or near the same area) can occur in up to 80% of EPP patients. This rate drops to 13% when patients receive radiation therapy after surgery. But recurrence at distant sites can affect up to 55% of patients.
Other risks of EPP for mesothelioma include blood clots, heart problems and pneumonia. Long-term risks can include shortness of breath. This might lead to needing an oxygen tank or a mechanical respirator for a while after surgery.
Common Short-Term EPP Risks
Reconstruction of the diaphragm and pericardium carries an increased risk of incisional hernias. These hernias occur when abdominal organs protrude into the chest cavity, often resulting from a diaphragm that has not been properly secured.
It’s important to watch for signs of serious issues that may develop after an EPP. These signs include fever, chest pain, cough and shortness of breath. They may signal life-threatening complications. A fever might indicate a developing empyema (pus buildup behind the patch used in reconstruction) and a cough could point to a bronchopleural fistula, where the airway leaks into the chest cavity. If you notice any of these symptoms or if your incision becomes red, swollen, painful or begins to ooze blood, please contact your doctor immediately.
Recovering from an EPP can take some time. Healing happens in phases. It also gets easier with time when you follow the guidance of your medical team.
After an EPP, the body undergoes significant change as it adapts to having one lung removed. The remaining lung expands to take up more room; the heart and central chest area shift slightly toward the side where the operation was performed; and fluid slowly fills the empty space in the chest.
It’s common for patients to have a harder time taking deep breaths and get tired more quickly. Many people can get back to their everyday daily lives after undergoing breathing exercises, physical therapy and paying close attention to potential issues like the shift of the chest organs or fluid buildup in the lungs.
Michael Cole tells us recovery from his EPP was challenging. But he credits the surgery with his long-term survival.
He shares, “When I woke up, I felt like I had been run over by a truck, and I’m pretty sure I looked worse. My whole body was out of whack, including my remaining lung. It hasn’t been easy, and we have been through hard times and uncertainty since that day but don’t misunderstand. We have not been in despair.”
The prognosis after EPP depends on your age, overall health, cancer stage, cell type and whether your surgeon was able to remove all tumors. Lymph node involvement is one of the most important factors. More cancer in the lymph nodes lowers the success rate of EPP.
A 2024 review of EPP for pleural mesothelioma reported a median survival of 18 months. The longest survival reached 35 months. But there are some patients who live longer. For example, Michael Cole’s EPP surgery was 10 years ago.
Additional therapies can improve prognosis after EPP. The National Comprehensive Cancer Network advises chemo before surgery based on clinical trial evidence. Postoperative chemo is also recommended for those who didn’t receive chemo before surgery. Combining treatments provides the best chance for improved survival.

Michael Cole
10-Year Pleural Survivor Undergoes Aggressive EPP Surgery
Michael Cole describes how aggressive EPP treatment for mesothelioma saved his life. He also explains his personal cancer journey and his other mesothelioma treatments.
Michael Cole
In the first six weeks following an EPP, a respiratory therapist helps rebuild breathing strength and lung function using a structured rehabilitation program. This program uses breathing tools, walking, deep-breathing exercises and regular check-ins with the respiratory therapist. Before attempting these steps on your own, talk to your doctor.
Weeks 1-2:
Weeks 3-4:
Weeks 5-6:
This process is a general guideline and should be tailored by your medical and rehab team based on your specific situation. Staying consistent with breathing exercises, mobility and therapy will help you make meaningful progress during this recovery period.

Hear from one of the nation’s top thoracic surgeons about how surgery can be effective for certain people with pleural mesothelioma.
Reserve Your SpotWithin the mesothelioma medical community, opinions vary about the value of EPP compared to other surgeries. Some experts believe EPP helps certain patients, while others think P/D is safer and just as effective.
A 2022 study found EPP and P/D had similar long-term outcomes when used as part of a larger treatment plan. However, EPP showed higher rates of mortality after surgery. The study recommends patients choose the safest treatment they can handle.
In our survey of mesothelioma surgeons, nearly 67% reported extrapleural pneumonectomy as yielding the best overall outcomes for eligible pleural mesothelioma patients, while 33% favored pleurectomy/decortication (P/D). Both surgeries can play an important role depending on the patient’s stage of cancer, overall health and surgical goals. These findings reflect how expert perspectives differ when tailoring treatment plans for individual patients.
The National Comprehensive Cancer Network says cell type, cancer stage, overall health and how much surgical risk a patient can accept should guide whether a patient receives EPP or P/D. A patient’s lung function and the surgeon’s skill and experience are also important considerations.
| Metric | EPP (Extrapleural Pneumonectomy) | P/D (Pleurectomy/Decortication) |
|---|---|---|
| Median overall survival | 15 months | 22 months |
| Risk of death during or shortly after surgery | 4% to 5% short-term death rate | 1% to 2% short-term death rate |
| Long-term quality of life benefit | In one study, physical/social/pain-related improvements lasted longer with EPP. | P/D showed earlier improvement in symptoms, but with a shorter duration in that study. |
| Risk of cancer returning (recurrence rate) | Lower local recurrence (33%) reported in one study. | Higher recurrence (65%) reported in the same study. |
The potential cost of an extrapleural pneumonectomy is around $82,000. This typically covers major charges like the surgeon’s fee, hospital stay (including ICU care), anesthesia services, synthetic materials (for diaphragm and pericardium reconstruction), and initial chemotherapy. This estimate can vary greatly throughout the U.S. It’s based on a 2019 report about the cost of mesothelioma treatment, and it accounts for inflation.
It does not account for many out-of-pocket expenses such as long-term physical therapy or pulmonary rehab, travel and lodging for treatment, home health care, nutritional supplements or lost income.
EPP patients can prepare for the procedure by improving their overall health. A balanced diet, gentle exercise and good sleep prepare the body for aggressive surgery. Preoperative pulmonary rehabilitation may be recommended. Quitting smoking will improve the function of the remaining lung after the procedure. Mental preparation may include counseling, joining support groups and learning about the procedure and recovery process.
After surgery, EPP patients get follow-up care, physical therapy and pain management. Pain relief starts in the operating room with pain medications given through a thoracic epidural catheter or another method. Over the next couple of days, pain meds are given via IV before switching to oral medications. From there, rehabilitation continues with physical and respiratory therapy, guidance from a dietitian on nutrition for recovery, and access to financial assistance programs to help cover treatment-related costs.
Other treatments for mesothelioma include immunotherapy, chemotherapy and radiation. Oncologists also use targeted therapies and Tumor Treating Fields therapy to treat mesothelioma.
Stay up-to-date on treatment, research, clinical trials, doctors and survivors
The information on this website is proprietary and protected. It is not a substitute for professional medical advice, diagnosis or treatment. Any unauthorized or illegal use, copying or dissemination will be prosecuted. Please read our privacy policy and terms of service for more information about our website.
This website and its content may be deemed attorney advertising. Prior results do not predict a similar outcome.
The Mesothelioma Center’s claim as the most trusted resource is based on our more than 150 5-star Google and BBB reviews. Our organization also helps more than half of all mesothelioma patients annually diagnosed.
Your web browser is no longer supported by Microsoft. Update your browser for more security, speed and compatibility.
If you are looking for mesothelioma support, please contact our Patient Advocates at (855) 404-4592
The Mesothelioma Center at Asbestos.com has provided patients and their loved ones the most updated and reliable information on mesothelioma and asbestos exposure since 2006.
Our team of Patient Advocates includes a medical doctor, a registered nurse, health services administrators, veterans, VA-accredited Claims Agents, an oncology patient navigator and hospice care expert. Their combined expertise means we help any mesothelioma patient or loved one through every step of their cancer journey.
More than 30 contributors, including mesothelioma doctors, survivors, health care professionals and other experts, have peer-reviewed our website and written unique research-driven articles to ensure you get the highest-quality medical and health information.
My family has only the highest compliment for the assistance and support that we received from The Mesothelioma Center. This is a staff of compassionate and knowledgeable individuals who respect what your family is experiencing and who go the extra mile to make an unfortunate diagnosis less stressful. Information and assistance were provided by The Mesothelioma Center at no cost to our family.LashawnMesothelioma patient’s daughter


Asbestos.com. (2026, February 18). Extrapleural Pneumonectomy. Retrieved March 5, 2026, from https://www.asbestos.com/treatment/surgery/extrapleural-pneumonectomy/
"Extrapleural Pneumonectomy." Asbestos.com, 18 Feb 2026, https://www.asbestos.com/treatment/surgery/extrapleural-pneumonectomy/.
Asbestos.com. "Extrapleural Pneumonectomy." Last modified February 18, 2026. https://www.asbestos.com/treatment/surgery/extrapleural-pneumonectomy/.

Thoracic surgeon Dr. Nestor Villamizar leads the multidisciplinary program at Sylvester Comprehensive Cancer Center.
Our fact-checking process begins with a thorough review of all sources to ensure they are high quality. Then we cross-check the facts with original medical or scientific reports published by those sources, or we validate the facts with reputable news organizations, medical and scientific experts and other health experts. Each page includes all sources for full transparency.
Please read our editorial guidelines to learn more about our content creation and review process.
