Based on Your Reading:
Get a Mesothelioma Treatment Guide

Find a Top Mesothelioma Doctor

Access Help Paying for Treatment

Written by Karen Selby, RN | Medically Reviewed By Dr. Andrea Wolf | Edited By Walter Pacheco | Last Update: July 2, 2024
Pleurectomy/decortication (P/D) surgery is a two-part procedure. The pleurectomy involves opening the chest cavity and removing the pleural lining around the lung, as well as other cancerous tissues. The decortication then removes any visible tumor masses from the surface of the lung and the rest of the chest area.
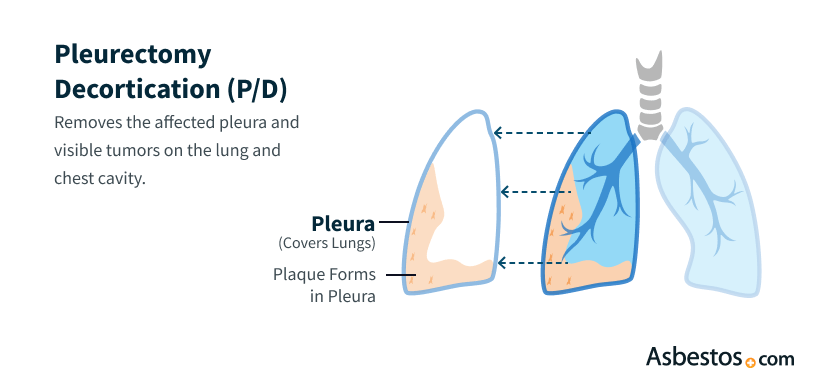
Pleurectomy/decortication surgery is an effective treatment for mesothelioma located in the lining of the lung, also called pleural mesothelioma. Removing the pleural tissue and any other cancerous growths in the lung can extend survival and significantly increase quality of life.
P/D surgery is most effective when it’s part of a comprehensive treatment approach. Studies show that this kind of multimodal approach can increase survival rates. Surgeons use postoperative chemotherapy, radiation therapy or immunotherapy to eliminate any remaining cancer cells. In addition, using adjuvant therapies can prevent or delay cancer recurrence.
The pleurectomy portion (also known as a parietal pleurectomy) of P/D surgery involves opening the chest cavity and removing the outside layer of the lining of the lungs. It removes all visible cancerous tissue. It typically takes between 2 and 4 hours.
At the beginning of surgery, the team carefully positions the patient on their side. To access the chest cavity, the surgeon makes a long incision along the back called a thoracotomy. The incision begins near the top of the ribcage and runs parallel to the spine before extending outward near the bottom of the ribcage.
Pleurectomy is a lung-sparing operation that takes out the lining of the pleura as well as, potentially, the diaphragm and the pericardium.
If there is cancer in the lower chest, the surgeon may perform a second incision to reach that area of the chest cavity. In some cases, surgeons remove the sixth rib to access the entire chest cavity.
The surgeon then removes the parietal pleura, which is the outside layer of the pleural lining. The surgeon will also remove other cancerous tissues, including any present on the chest wall lining, heart sac or diaphragm.
Get a Mesothelioma Treatment Guide

Find a Top Mesothelioma Doctor

Access Help Paying for Treatment

Decortication is a surgical procedure used to remove cancerous or abnormal tissue on the lungs, chest wall or diaphragm. The surgeon typically performs this procedure after finishing the parietal pleurectomy. The surgeon removes any visible tumor growth and may surgically scrape the lung to ensure the removal of any malignant tissue.
We’re finding that we’re able to remove all the tumor that’s visible. That’s why there’s been a shift toward doing this lung-sparing procedure more so than in decades past.
As the surgical team completes the procedure, they’ll take steps to prevent postoperative bleeding, such as suturing or cauterizing blood vessels. Some specialists have also integrated experimental targeted treatments such as photodynamic therapy, heated intrapleural chemotherapy or chemotherapy gels, which have shown promising results.
The final step is for the surgeon to stitch the incision closed. The decortication portion of a P/D takes about 2 to 3 hours.
Kevin Hession underwent decortication surgery to remove all visible tumors in January 2022, about 5 months after being diagnosed with pleural mesothelioma. Kevin spoke with The Mesothelioma Center to share his experiences while recovering from surgery and to explain some lasting effects from the procedure.
Not all people with a mesothelioma diagnosis are eligible for P/D. Surgeons assess each individual to make sure that P/D is the appropriate treatment.
P/D can treat early-stage (stage 1 or 2) pleural mesothelioma. In these stages, the cancer is confined to the chest cavity and hasn’t spread to other areas of the body, so surgery can remove all cancerous tissue.
Individuals who are eligible for P/D may also benefit from additional therapies. These may include chemotherapy or radiation to further destroy cancer cells and prevent the progression or recurrence of disease.
Like any surgery, P/D offers benefits and risks. The procedure has a good record of reducing mesothelioma symptoms and prolonging life. However, complications are a possible risk.
While some surgeons debate the pros and cons of P/D versus the more invasive extrapleural pneumonectomy (EPP) procedure, research studies show P/D can lead to longer survival. Because it’s associated with fewer complications and better quality of life, with only 1% to 2% of patients dying during or immediately after the surgery, most mesothelioma specialists today agree that P/D is preferable in cases where cancer tissue has not invaded the lung.
Findings presented in 2023 raised questions about the efficacy of P/D and chemotherapy compared with chemotherapy alone. The study showed that chemotherapy alone may offer better outcomes than chemotherapy with surgery. The subject will require further study, and individuals should discuss all treatment options with their mesothelioma care team.

Receive a free recording of our webinar for expert tips on managing the side effects of surgery and other top mesothelioma treatments.
Get a RecordingThe first step in planning for P/D surgery is the surgical consultation. This meeting ensures that the patient and their loved ones understand what will happen before, during and after surgery.
Patients may meet in person or virtually with the surgeon and the surgical team. They can ask detailed questions, bring up concerns and inquire about the surgeon’s success rate.
Related Videos:
Most individuals require a hospital stay of about 2 weeks after P/D, so doctors monitor recovery closely. The staff can identify signs of complications such as infection, pneumonia or bleeding and take appropriate action. The care team can use the time to teach patients deep-breathing exercises and other therapies to aid recovery.
Total recovery from surgery usually takes several more weeks after hospital discharge. The care team will provide detailed instructions on how to continue recovery at home and arrange for any necessary visits from occupational and pulmonary therapists. Some patients may be eligible for complementary therapies, such as pulmonary rehabilitation. Following care instructions and attending follow-up appointments will safeguard patient health.
Pleurectomy and decortication have a 90% success rate in reducing symptoms and can increase survival time to about 20 months. It’s not considered a cure for mesothelioma, but this surgery is among the most effective treatment options when combined with a multimodal mesothelioma treatment approach.
The median survival after P/D is about 20 months, depending on other prognostic factors, such as the stage of mesothelioma, treatment approach and patient health status. Multimodal treatment protocols may improve survival rates.
Thoracic surgeon Dr. Robert Cameron, a mesothelioma specialist from UCLA Medical Center, pioneered the P/D surgery more than 20 years ago. Before that, a pleurectomy was commonly performed as a palliative measure for pleural mesothelioma patients because it reduced the buildup of fluid around a lung and alleviated pain. Surgical advancements in decortication and Dr. Cameron’s work led to pairing the two procedures.
Dr. Cameron is the driving force behind the Pacific Mesothelioma Center and has campaigned to make P/D the standard of care for early-stage pleural mesothelioma.
Thank you for your feedback. Would you like to speak with a Patient Advocate?
Your web browser is no longer supported by Microsoft. Update your browser for more security, speed and compatibility.
If you are looking for mesothelioma support, please contact our Patient Advocates at (855) 404-4592
The Mesothelioma Center at Asbestos.com has provided patients and their loved ones the most updated and reliable information on mesothelioma and asbestos exposure since 2006.
Our team of Patient Advocates includes a medical doctor, a registered nurse, health services administrators, veterans, VA-accredited Claims Agents, an oncology patient navigator and hospice care expert. Their combined expertise means we help any mesothelioma patient or loved one through every step of their cancer journey.
More than 30 contributors, including mesothelioma doctors, survivors, health care professionals and other experts, have peer-reviewed our website and written unique research-driven articles to ensure you get the highest-quality medical and health information.
My family has only the highest compliment for the assistance and support that we received from The Mesothelioma Center. This is a staff of compassionate and knowledgeable individuals who respect what your family is experiencing and who go the extra mile to make an unfortunate diagnosis less stressful. Information and assistance were provided by The Mesothelioma Center at no cost to our family.LashawnMesothelioma patient’s daughter


Selby, K. (2024, July 2). Pleurectomy/Decortication. Asbestos.com. Retrieved July 26, 2024, from https://www.asbestos.com/treatment/surgery/pleurectomy/
Selby, Karen. "Pleurectomy/Decortication." Asbestos.com, 2 Jul 2024, https://www.asbestos.com/treatment/surgery/pleurectomy/.
Selby, Karen. "Pleurectomy/Decortication." Asbestos.com. Last modified July 2, 2024. https://www.asbestos.com/treatment/surgery/pleurectomy/.
The Mesothelioma Center at Asbestos.com has provided patients and their loved ones the most updated and reliable information on mesothelioma and asbestos exposure since 2006.
Our team of Patient Advocates includes a medical doctor, a registered nurse, health services administrators, veterans, VA-accredited Claims Agents, an oncology patient navigator and hospice care expert. Their combined expertise means we help any mesothelioma patient or loved one through every step of their cancer journey.
More than 30 contributors, including mesothelioma doctors, survivors, health care professionals and other experts, have peer-reviewed our website and written unique research-driven articles to ensure you get the highest-quality medical and health information.
My family has only the highest compliment for the assistance and support that we received from The Mesothelioma Center. This is a staff of compassionate and knowledgeable individuals who respect what your family is experiencing and who go the extra mile to make an unfortunate diagnosis less stressful. Information and assistance were provided by The Mesothelioma Center at no cost to our family.LashawnMesothelioma patient’s daughter


Selby, K. (2024, July 2). Pleurectomy/Decortication. Asbestos.com. Retrieved July 26, 2024, from https://www.asbestos.com/treatment/surgery/pleurectomy/
Selby, Karen. "Pleurectomy/Decortication." Asbestos.com, 2 Jul 2024, https://www.asbestos.com/treatment/surgery/pleurectomy/.
Selby, Karen. "Pleurectomy/Decortication." Asbestos.com. Last modified July 2, 2024. https://www.asbestos.com/treatment/surgery/pleurectomy/.
The Mesothelioma Center at Asbestos.com has provided patients and their loved ones the most updated and reliable information on mesothelioma and asbestos exposure since 2006.
Our team of Patient Advocates includes a medical doctor, a registered nurse, health services administrators, veterans, VA-accredited Claims Agents, an oncology patient navigator and hospice care expert. Their combined expertise means we help any mesothelioma patient or loved one through every step of their cancer journey.
More than 30 contributors, including mesothelioma doctors, survivors, health care professionals and other experts, have peer-reviewed our website and written unique research-driven articles to ensure you get the highest-quality medical and health information.
My family has only the highest compliment for the assistance and support that we received from The Mesothelioma Center. This is a staff of compassionate and knowledgeable individuals who respect what your family is experiencing and who go the extra mile to make an unfortunate diagnosis less stressful. Information and assistance were provided by The Mesothelioma Center at no cost to our family.LashawnMesothelioma patient’s daughter


Selby, K. (2024, July 2). Pleurectomy/Decortication. Asbestos.com. Retrieved July 26, 2024, from https://www.asbestos.com/treatment/surgery/pleurectomy/
Selby, Karen. "Pleurectomy/Decortication." Asbestos.com, 2 Jul 2024, https://www.asbestos.com/treatment/surgery/pleurectomy/.
Selby, Karen. "Pleurectomy/Decortication." Asbestos.com. Last modified July 2, 2024. https://www.asbestos.com/treatment/surgery/pleurectomy/.
The Mesothelioma Center at Asbestos.com has provided patients and their loved ones the most updated and reliable information on mesothelioma and asbestos exposure since 2006.
Our team of Patient Advocates includes a medical doctor, a registered nurse, health services administrators, veterans, VA-accredited Claims Agents, an oncology patient navigator and hospice care expert. Their combined expertise means we help any mesothelioma patient or loved one through every step of their cancer journey.
More than 30 contributors, including mesothelioma doctors, survivors, health care professionals and other experts, have peer-reviewed our website and written unique research-driven articles to ensure you get the highest-quality medical and health information.
My family has only the highest compliment for the assistance and support that we received from The Mesothelioma Center. This is a staff of compassionate and knowledgeable individuals who respect what your family is experiencing and who go the extra mile to make an unfortunate diagnosis less stressful. Information and assistance were provided by The Mesothelioma Center at no cost to our family.LashawnMesothelioma patient’s daughter


Selby, K. (2024, July 2). Pleurectomy/Decortication. Asbestos.com. Retrieved July 26, 2024, from https://www.asbestos.com/treatment/surgery/pleurectomy/
Selby, Karen. "Pleurectomy/Decortication." Asbestos.com, 2 Jul 2024, https://www.asbestos.com/treatment/surgery/pleurectomy/.
Selby, Karen. "Pleurectomy/Decortication." Asbestos.com. Last modified July 2, 2024. https://www.asbestos.com/treatment/surgery/pleurectomy/.
The Mesothelioma Center at Asbestos.com has provided patients and their loved ones the most updated and reliable information on mesothelioma and asbestos exposure since 2006.
Our team of Patient Advocates includes a medical doctor, a registered nurse, health services administrators, veterans, VA-accredited Claims Agents, an oncology patient navigator and hospice care expert. Their combined expertise means we help any mesothelioma patient or loved one through every step of their cancer journey.
More than 30 contributors, including mesothelioma doctors, survivors, health care professionals and other experts, have peer-reviewed our website and written unique research-driven articles to ensure you get the highest-quality medical and health information.
My family has only the highest compliment for the assistance and support that we received from The Mesothelioma Center. This is a staff of compassionate and knowledgeable individuals who respect what your family is experiencing and who go the extra mile to make an unfortunate diagnosis less stressful. Information and assistance were provided by The Mesothelioma Center at no cost to our family.LashawnMesothelioma patient’s daughter


Selby, K. (2024, July 2). Pleurectomy/Decortication. Asbestos.com. Retrieved July 26, 2024, from https://www.asbestos.com/treatment/surgery/pleurectomy/
Selby, Karen. "Pleurectomy/Decortication." Asbestos.com, 2 Jul 2024, https://www.asbestos.com/treatment/surgery/pleurectomy/.
Selby, Karen. "Pleurectomy/Decortication." Asbestos.com. Last modified July 2, 2024. https://www.asbestos.com/treatment/surgery/pleurectomy/.
The Mesothelioma Center at Asbestos.com has provided patients and their loved ones the most updated and reliable information on mesothelioma and asbestos exposure since 2006.
Our team of Patient Advocates includes a medical doctor, a registered nurse, health services administrators, veterans, VA-accredited Claims Agents, an oncology patient navigator and hospice care expert. Their combined expertise means we help any mesothelioma patient or loved one through every step of their cancer journey.
More than 30 contributors, including mesothelioma doctors, survivors, health care professionals and other experts, have peer-reviewed our website and written unique research-driven articles to ensure you get the highest-quality medical and health information.
My family has only the highest compliment for the assistance and support that we received from The Mesothelioma Center. This is a staff of compassionate and knowledgeable individuals who respect what your family is experiencing and who go the extra mile to make an unfortunate diagnosis less stressful. Information and assistance were provided by The Mesothelioma Center at no cost to our family.LashawnMesothelioma patient’s daughter


Selby, K. (2024, July 2). Pleurectomy/Decortication. Asbestos.com. Retrieved July 26, 2024, from https://www.asbestos.com/treatment/surgery/pleurectomy/
Selby, Karen. "Pleurectomy/Decortication." Asbestos.com, 2 Jul 2024, https://www.asbestos.com/treatment/surgery/pleurectomy/.
Selby, Karen. "Pleurectomy/Decortication." Asbestos.com. Last modified July 2, 2024. https://www.asbestos.com/treatment/surgery/pleurectomy/.
The Mesothelioma Center at Asbestos.com has provided patients and their loved ones the most updated and reliable information on mesothelioma and asbestos exposure since 2006.
Our team of Patient Advocates includes a medical doctor, a registered nurse, health services administrators, veterans, VA-accredited Claims Agents, an oncology patient navigator and hospice care expert. Their combined expertise means we help any mesothelioma patient or loved one through every step of their cancer journey.
More than 30 contributors, including mesothelioma doctors, survivors, health care professionals and other experts, have peer-reviewed our website and written unique research-driven articles to ensure you get the highest-quality medical and health information.
My family has only the highest compliment for the assistance and support that we received from The Mesothelioma Center. This is a staff of compassionate and knowledgeable individuals who respect what your family is experiencing and who go the extra mile to make an unfortunate diagnosis less stressful. Information and assistance were provided by The Mesothelioma Center at no cost to our family.LashawnMesothelioma patient’s daughter


Selby, K. (2024, July 2). Pleurectomy/Decortication. Asbestos.com. Retrieved July 26, 2024, from https://www.asbestos.com/treatment/surgery/pleurectomy/
Selby, Karen. "Pleurectomy/Decortication." Asbestos.com, 2 Jul 2024, https://www.asbestos.com/treatment/surgery/pleurectomy/.
Selby, Karen. "Pleurectomy/Decortication." Asbestos.com. Last modified July 2, 2024. https://www.asbestos.com/treatment/surgery/pleurectomy/.
The Mesothelioma Center at Asbestos.com has provided patients and their loved ones the most updated and reliable information on mesothelioma and asbestos exposure since 2006.
Our team of Patient Advocates includes a medical doctor, a registered nurse, health services administrators, veterans, VA-accredited Claims Agents, an oncology patient navigator and hospice care expert. Their combined expertise means we help any mesothelioma patient or loved one through every step of their cancer journey.
More than 30 contributors, including mesothelioma doctors, survivors, health care professionals and other experts, have peer-reviewed our website and written unique research-driven articles to ensure you get the highest-quality medical and health information.
My family has only the highest compliment for the assistance and support that we received from The Mesothelioma Center. This is a staff of compassionate and knowledgeable individuals who respect what your family is experiencing and who go the extra mile to make an unfortunate diagnosis less stressful. Information and assistance were provided by The Mesothelioma Center at no cost to our family.LashawnMesothelioma patient’s daughter


Selby, K. (2024, July 2). Pleurectomy/Decortication. Asbestos.com. Retrieved July 26, 2024, from https://www.asbestos.com/treatment/surgery/pleurectomy/
Selby, Karen. "Pleurectomy/Decortication." Asbestos.com, 2 Jul 2024, https://www.asbestos.com/treatment/surgery/pleurectomy/.
Selby, Karen. "Pleurectomy/Decortication." Asbestos.com. Last modified July 2, 2024. https://www.asbestos.com/treatment/surgery/pleurectomy/.
The Mesothelioma Center at Asbestos.com has provided patients and their loved ones the most updated and reliable information on mesothelioma and asbestos exposure since 2006.
Our team of Patient Advocates includes a medical doctor, a registered nurse, health services administrators, veterans, VA-accredited Claims Agents, an oncology patient navigator and hospice care expert. Their combined expertise means we help any mesothelioma patient or loved one through every step of their cancer journey.
More than 30 contributors, including mesothelioma doctors, survivors, health care professionals and other experts, have peer-reviewed our website and written unique research-driven articles to ensure you get the highest-quality medical and health information.
My family has only the highest compliment for the assistance and support that we received from The Mesothelioma Center. This is a staff of compassionate and knowledgeable individuals who respect what your family is experiencing and who go the extra mile to make an unfortunate diagnosis less stressful. Information and assistance were provided by The Mesothelioma Center at no cost to our family.LashawnMesothelioma patient’s daughter


Selby, K. (2024, July 2). Pleurectomy/Decortication. Asbestos.com. Retrieved July 26, 2024, from https://www.asbestos.com/treatment/surgery/pleurectomy/
Selby, Karen. "Pleurectomy/Decortication." Asbestos.com, 2 Jul 2024, https://www.asbestos.com/treatment/surgery/pleurectomy/.
Selby, Karen. "Pleurectomy/Decortication." Asbestos.com. Last modified July 2, 2024. https://www.asbestos.com/treatment/surgery/pleurectomy/.
The Mesothelioma Center at Asbestos.com has provided patients and their loved ones the most updated and reliable information on mesothelioma and asbestos exposure since 2006.
Our team of Patient Advocates includes a medical doctor, a registered nurse, health services administrators, veterans, VA-accredited Claims Agents, an oncology patient navigator and hospice care expert. Their combined expertise means we help any mesothelioma patient or loved one through every step of their cancer journey.
More than 30 contributors, including mesothelioma doctors, survivors, health care professionals and other experts, have peer-reviewed our website and written unique research-driven articles to ensure you get the highest-quality medical and health information.
My family has only the highest compliment for the assistance and support that we received from The Mesothelioma Center. This is a staff of compassionate and knowledgeable individuals who respect what your family is experiencing and who go the extra mile to make an unfortunate diagnosis less stressful. Information and assistance were provided by The Mesothelioma Center at no cost to our family.LashawnMesothelioma patient’s daughter


Selby, K. (2024, July 2). Pleurectomy/Decortication. Asbestos.com. Retrieved July 26, 2024, from https://www.asbestos.com/treatment/surgery/pleurectomy/
Selby, Karen. "Pleurectomy/Decortication." Asbestos.com, 2 Jul 2024, https://www.asbestos.com/treatment/surgery/pleurectomy/.
Selby, Karen. "Pleurectomy/Decortication." Asbestos.com. Last modified July 2, 2024. https://www.asbestos.com/treatment/surgery/pleurectomy/.
A medical doctor who specializes in mesothelioma or cancer treatment reviewed the content on this page to ensure it meets current medical standards and accuracy.
Please read our editorial guidelines to learn more about our content creation and review process.
Dr. Andrea Wolf is the Director of the New York Mesothelioma Program at Mount Sinai in New York City. She focuses on multidisciplinary treatment, clinical research, community outreach and education.
A medical doctor who specializes in mesothelioma or cancer treatment reviewed the content on this page to ensure it meets current medical standards and accuracy.
Please read our editorial guidelines to learn more about our content creation and review process.
Dr. Andrea Wolf is the Director of the New York Mesothelioma Program at Mount Sinai in New York City. She focuses on multidisciplinary treatment, clinical research, community outreach and education.
Mesothelioma Center - Vital Services for Cancer Patients & Families doesn’t believe in selling customer information. However, as required by the new California Consumer Privacy Act (CCPA), you may record your preference to view or remove your personal information by completing the form below.
