Get Your Free Mesothelioma Guide

Find a Top Mesothelioma Doctor

Access Help Paying for Treatment

Asbestosis can cause a dry cough, shortness of breath and swelling in the face or neck. These symptoms often appear decades after exposure, which makes diagnosis challenging. Doctors rely on your medical history, physical exam and imaging tests to confirm asbestosis and plan your care.

People with asbestosis may notice symptoms like trouble breathing, a dry cough or a feeling of tightness in the chest. These problems happen when asbestos fibers settle in the lungs and cause scarring. Over time, this scarring makes it harder for the lungs to work well.
Asbestosis symptoms often take 10 to 40 years to appear and may look like other lung diseases, such as COPD or pulmonary fibrosis. They usually get worse over time and can also show up in other asbestos-related conditions, including pleural mesothelioma and lung cancer. If you’ve been exposed to asbestos and notice these signs, talk to your doctor about your risk for asbestosis to ensure a timely and accurate diagnosis.
Common Asbestosis Symptoms
Navy veteran Jerry Cochran tells us he was initially diagnosed with sarcoidosis in 1975, but when his symptoms began to change, he wanted to find answers. The more he read about his symptoms, the more he felt they didn’t match up with his diagnosis. Jerry says, “Armed with that information, I knew that something was going on. “And that made me even more curious about this disease.”
Eventually he was diagnosed with silicosis in 1991. But he began to feel his worsening symptoms meant something else was going on. In 2010, nearly 20 years after his silicosis diagnosis and 35 years after his sarcoidosis diagnosis, he received an asbestosis diagnosis.
Asbestosis symptoms can be a sign of complications or other serious conditions. Although asbestosis itself isn’t cancerous, long-term asbestos exposure is known to cause cancer and other life-threatening complications.
Conditions Associated With Asbestosis
Although mesothelioma and asbestosis are both the result of asbestos exposure, one condition isn’t a direct complication of the other. However, developing one asbestos-related disease can indicate a higher likelihood of developing another.
Symptoms of asbestosis tend to appear slowly, 20 to 30 years after exposure, and become more severe over time. In the early stages, symptoms may be mild and easy to ignore. As the disease progresses, inflammation and scarring make breathing more difficult, which can have a significant impact on daily life.
Asbestos fibers are tiny, sharp and straight. When people breathe them in, the fibers can get stuck in the lungs. The body has a hard time pushing them out. Over decades, the damage to the lungs can be irreversible and even deadly.
| Stage | Early Symptoms | Late Symptoms |
|---|---|---|
| Onset | Shortness of breath during physical activity | Difficulty breathing even at rest |
| Respiratory | Mild, dry cough | Persistent, dry cough with chest tightness |
| Physical | General fatigue or reduced exercise tolerance | Clubbing of the fingers, chest pain |
Although there is no cure for asbestosis, many treatment strategies can help relieve asbestosis symptoms and improve quality of life. People may benefit from palliative care or personalized asbestosis treatment options based on the severity of symptoms and overall health.
Ways to Manage Asbestosis Symptoms
These asbestosis treatment options aren’t one-size-fits-all. The best way to treat asbestosis symptoms depends on your health. The goal is to make your quality of life better and slow the disease. Regular check-ups and prescribed medicines can help. Acting early and talking with your care team can help control symptoms and prevent more problems.
Get Your Free Mesothelioma Guide

Find a Top Mesothelioma Doctor

Access Help Paying for Treatment

Asbestosis is diagnosed with a discussion of your asbestos exposure history, lung function tests and imaging scans. Doctors take your asbestos exposure history into account when reviewing your test results when making a diagnosis.
Tests to identify asbestosis and other forms of lung fibrosis look for certain signs and symptoms. Examples include crackling breathing sounds, scar tissue in the lungs and pleural plaque buildup.
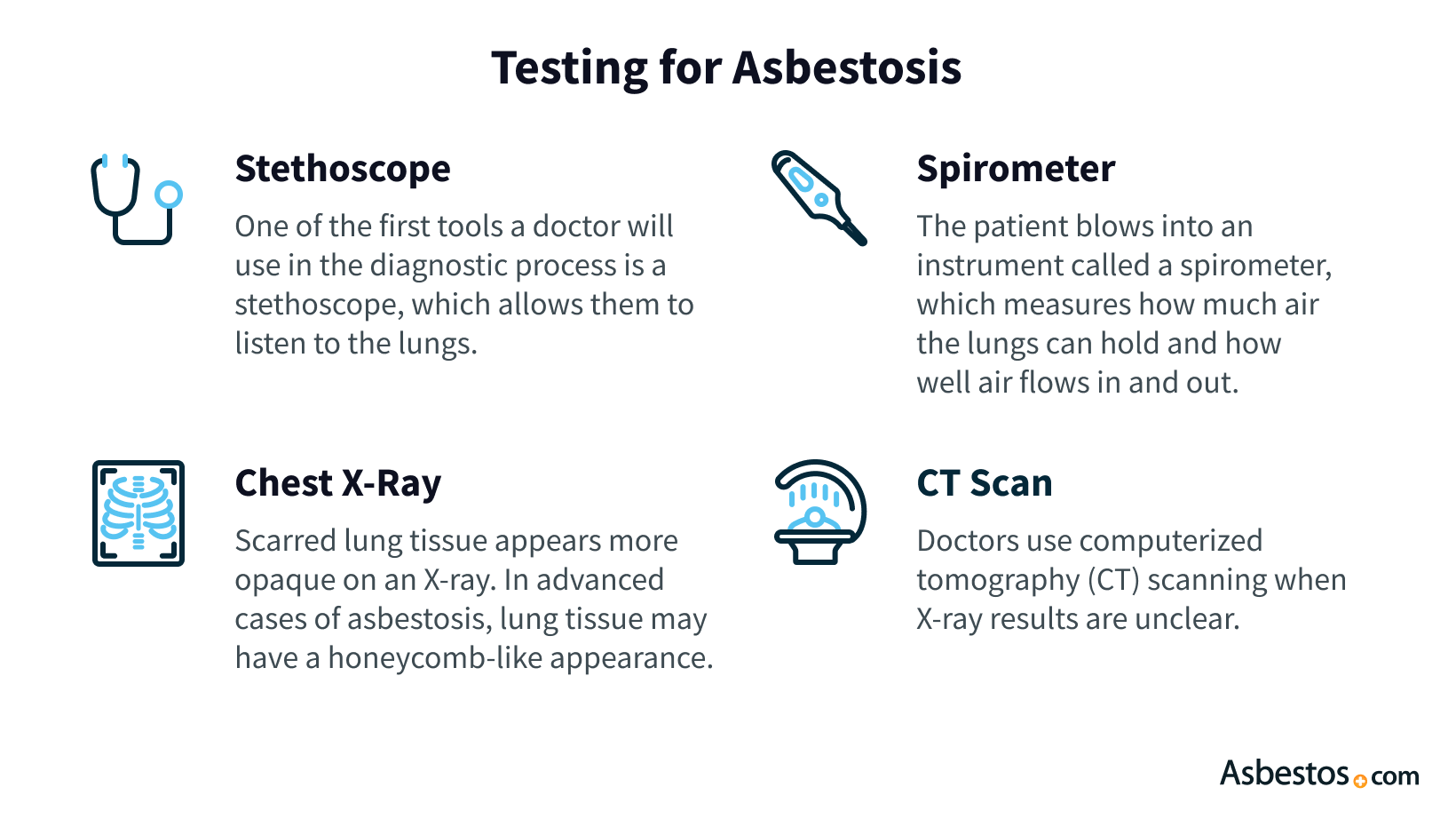
Discussing exposure to asbestos at work or home can indicate to your doctor that asbestosis could be a possible diagnosis. Jobs such as construction, shipbuilding or manufacturing have higher exposure risks. During an exam, your doctor may hear crackling in your lungs, observe changes in your fingers or notice breathing difficulties.
Your history of exposure helps your doctor decide what tests to do. If you’ve worked with asbestos or lived with someone who has, share this info with your doctor.
Imaging is key to diagnosing asbestosis. Chest X-rays and CT scans are used to find signs like pleural plaques or lung scarring. These images can show asbestos fibers have damaged your lungs.
Imaging also helps rule out other lung problems with similar symptoms. CT scans give more detailed pictures of your lungs and can find changes that X-rays might miss.
Pulmonary function tests can detect reduced airflow, decreased lung volume and lower oxygen exchange associated with asbestosis. PFTs may include a lung capacity test, respiratory muscle strength and performance tests for mild cardio, such as a 6-minute walk.
PFTs are helpful for checking if asbestosis is getting worse and whether treatments are working. The results help doctors choose the next steps to manage symptoms.
A lung biopsy is sometimes done to check for asbestosis, especially if scans and breathing tests don’t give a clear answer. Doctors take a small piece of lung tissue and look at it under a microscope for signs of scarring and asbestos fibers.
Doctors can see damage from asbestos fibers in the lung tissue. A biopsy is more common if there is concern about other problems, such as mesothelioma or lung cancer.

Get a free guide with the latest mesothelioma treatments and clinical trials.
Get Yours NowBecause asbestosis symptoms develop slowly and can look like other lung problems, finding it early is very important. Detecting the disease early can help prevent serious issues and make it easier to manage symptoms.
It can take 20 to 30 years after being exposed to asbestos for asbestosis to be diagnosed. If you notice symptoms like shortness of breath, frequent cough or chest pain, especially if you have a history of asbestos exposure, see a doctor right away.
When you have asbestosis, your doctor will give your condition a grade from 0 to 4. Grade 0 is the lowest, and grade 4 is the highest. Knowing what each grade means is important because it helps guide your treatment.
The 5 Grades of Asbestosis
Usually, the amount of scarring in your lungs determines the grade of your asbestosis. More scarring means a worse case, which needs stronger treatment.
Jerry Cochran felt like something else was going on since his condition was worsening. He was then diagnosed with asbestosis. He struggles to breathe because his lungs can’t expand and contract the way they’re supposed to. The paint he scraped off of the aircraft carrier he served on decades ago contained asbestos, leading to his asbestosis. The condition is incurable, but many patients can survive several decades with treatment.
After being diagnosed with asbestosis, it’s important to take steps to protect your health and prevent symptoms from worsening. The first and most crucial step after receiving an asbestosis diagnosis is to avoid any further asbestos exposure. While the condition is incurable, treatment for asbestosis can help reduce its impact.
Next Steps After an Asbestosis Diagnosis
Once you’re no longer exposed to asbestos, simple changes like eating healthy and doing moderate cardio can help control asbestosis symptoms. Having a plan helps to manage asbestosis symptoms and reduces the chance of more problems. Your health care team will help you develop a treatment plan with tailored advice based on your needs.
No, asbestosis can’t be cured. However, treatments such as pain medication and pulmonary rehab can relieve symptoms, slow progression and improve quality of life.
Asbestosis is a lung disease that isn’t cancerous. Mesothelioma is a rare and fast-growing cancer. Asbestos exposure causes both asbestosis and mesothelioma, but each disease has different outcomes and ways to treat them.
If you think you have asbestosis, see a doctor immediately, especially if you’ve had past asbestos exposure. Early diagnosis can help reduce complications and lead to better treatment outcomes.
Because asbestosis can look like other lung problems, doctors might mistake it for something else. Misdiagnosis can delay treatment while your asbestosis symptoms worsen. A second opinion can help make sure you have asbestosis and not a different condition.
Your web browser is no longer supported by Microsoft. Update your browser for more security, speed and compatibility.
If you are looking for mesothelioma support, please contact our Patient Advocates at (855) 404-4592
The Mesothelioma Center at Asbestos.com has provided patients and their loved ones the most updated and reliable information on mesothelioma and asbestos exposure since 2006.
Our team of Patient Advocates includes a medical doctor, a registered nurse, health services administrators, veterans, VA-accredited Claims Agents, an oncology patient navigator and hospice care expert. Their combined expertise means we help any mesothelioma patient or loved one through every step of their cancer journey.
More than 30 contributors, including mesothelioma doctors, survivors, health care professionals and other experts, have peer-reviewed our website and written unique research-driven articles to ensure you get the highest-quality medical and health information.
My family has only the highest compliment for the assistance and support that we received from The Mesothelioma Center. This is a staff of compassionate and knowledgeable individuals who respect what your family is experiencing and who go the extra mile to make an unfortunate diagnosis less stressful. Information and assistance were provided by The Mesothelioma Center at no cost to our family.LashawnMesothelioma patient’s daughter


Asbestos.com. (2025, July 9). Asbestosis Symptoms and Diagnosis. Retrieved July 10, 2025, from https://www.asbestos.com/asbestosis/symptoms/
"Asbestosis Symptoms and Diagnosis." Asbestos.com, 9 Jul 2025, https://www.asbestos.com/asbestosis/symptoms/.
Asbestos.com. "Asbestosis Symptoms and Diagnosis." Last modified July 9, 2025. https://www.asbestos.com/asbestosis/symptoms/.
Arti Shukla, Ph.D., is an internationally renowned asbestos researcher known for her achievements in identifying biomarkers that cause mesothelioma. She is the director of the Shukla Research Lab, as well as a professor of pathology at The University of Vermont Larner College of Medicine.
Our fact-checking process begins with a thorough review of all sources to ensure they are high quality. Then we cross-check the facts with original medical or scientific reports published by those sources, or we validate the facts with reputable news organizations, medical and scientific experts and other health experts. Each page includes all sources for full transparency.
Please read our editorial guidelines to learn more about our content creation and review process.
