Lymphohistiocytoid Mesothelioma
Lymphohistiocytoid mesothelioma is a rare subtype of asbestos cancer that makes up less than 1% of all asbestos-related cancer cases. Tumors are made up of a dense bundle of inflammatory immune cells, including lymphocytes (a type of white blood cell), plasma cells and immobile immune cells called histiocytes or macrophages.
What Is Lymphohistiocytoid Mesothelioma?
Lymphohistoicytoid mesothelioma is an aggressive sarcomatoid cell type. These tumors tend to have a mix of epithelioid cells and inflammatory cells. Some patients with this subtype may have an optimistic prognosis, like an epithelial cell diagnosis.
There are few reported cases of this subtype. Doctors often misdiagnose it as another condition, which is often non-Hodgkin’s lymphoma. Symptoms and treatment options mirror those of other pleural mesothelioma types.
Its rarity leaves researchers few opportunities to study it, and there is little information for review. Pathologists have identified specific tumor characteristics that can aid in an accurate diagnosis.
- First discovered in 1988.
- Characterized by dense bundles of inflammatory and immune cells.
- Sarcomatoid cell type, mixed with some epithelioid.
- May be misdiagnosed as lymphoma.
- Treated with immunotherapy, chemotherapy and radiation therapy.
Diagnosing Lymphohistiocytoid Mesothelioma
First, surgeons take a sample of the tumor during a biopsy. Then, they send it to a lab for a pathological study. Many of the immune cells found in this subtype mimic other cancers. This can lead to misdiagnosis.
Differential Diagnoses of Lymphohistiocytoid Mesothelioma
- Non-Hodgkin’s lymphoma
- Hodgkin’s lymphoma
- Lymphoepithelial carcinoma
- Sarcomatoid carcinoma of the lung
- Ganglioneuroma
- Pleural-based thymic epithelial tumor
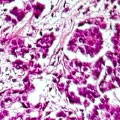
Under a microscope, histological studies reveal large, atypical polygonal to spindle-shaped histiocytoid cells. Mixed with these cells are white blood cells. Other signs of this tumor type include Diffuse pleural thickening, small nodules throughout the lining of the lung, and pleural effusion.
In immunohistochemistry, pathologists add antibodies to tumor tissue. These stain the tissue when there is a positive reaction. Each cancer has certain positive markers. Seeing them under a microscope can help make a more accurate diagnosis.
To prepare a sample, the pathologist fixes tumor tissue in a paraffin block. They then trim the block into thin slices and mount them on a slide. In studies, these tumor cells expressed cytokeratin, vimentin, calretinin and CH5/6. They were negative for lymphoid and macrophage markers. AE1/AE3 and calretinin antibodies are the most reliable for staining tissue samples.

Understand your diagnosis, top doctors and ways to afford care.
Get Your Free GuideSymptoms of Lymphohistiocytoid Mesothelioma
The symptoms of lymphohistoicytoid mesothelioma include chest pain, breathing problems, weight loss and fatigue. Symptoms of mesothelioma depend on the primary location of the tumors rather than the cell type. Symptoms of this type remain the same as other types of pleural mesothelioma.
- Chest pain or abdominal fullness
- Coughing up blood
- Fatigue and extreme tiredness
- Lack of appetite, anorexia and nausea
- Low blood oxygen levels
- Persistent cough
- Prolonged hoarseness
- Shortness of breath
- Weight loss and weakness
If you’re experiencing symptoms, it’s important to consult with a specialist. For those with a history of asbestos exposure, discussing cancer screening with your doctor may help. Early detection can open up more treatment avenues, potentially offering better outcomes.
Treatment and Prognosis of Lymphohistiocytoid Mesothelioma
Treatment information is limited for this type because of its rarity. Doctors may recommend immunotherapy, chemotherapy and radiation therapy. In general, surgery may not be recommended because lymphohistoicytoid mesothelioma is considered part of the sarcomatoid cell type, which tends to recur quickly.
A 2007 study evaluated 22 cases. This study showed improvement and a positive response to treatment. Patients had extended life spans. Their survival ranged between 32 and 40 months after diagnosis. Early cases in a 1988 report showed no positive response to chemotherapy or radiation. The three patients in the report survived between four and eight months.
One encouraging case study showed a spontaneous regression of the tumor. Doctors removed tumors from the patient via surgery. The patients remained alive and without symptoms for 12 years after the initial presentation. In limited studies, some patients survived as much as six years after diagnosis. Doctors suggest that immune cells in this tumor may contribute to spontaneous regression.
Recommended Reading



