
Connect with top-rated doctors specializing in mesothelioma treatment, who will personalize treatment options based on your diagnosis.
Find Your DoctorPericardial effusion is the main symptom of pericardial mesothelioma. Infections, inflammation and other cancers can also cause the fluid buildup seen in pericardial effusion. This buildup puts pressure on the heart and may lead to heart failure.
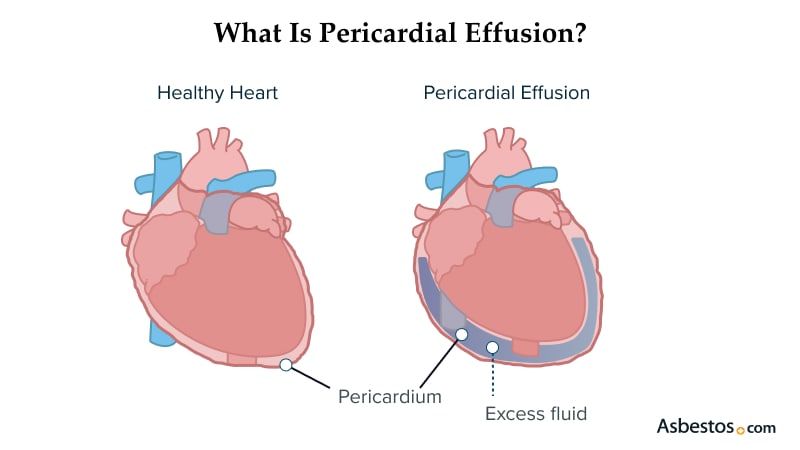
Mesothelioma-associated pericardial effusion happens when too much fluid builds up in the heart sac or the membranes covering your heart called the pericardium. The extra fluid in this space creates pressure on your heart and can become fatal.
Pericardial effusion is rare. This fluid can build up when the lining of your heart sac becomes irritated or inflamed. It can also happen if injury, surgery or disease causes blood or other fluids to enter the space.
Key Facts About Pericardial Effusions
Treatment needs to start as soon as symptoms are detected. The aim of treatment is to relieve pressure on the heart and treat the underlying cause. Doctors can offer tailored approaches based on symptoms and causes. Staying aware of symptoms can help you begin treatment before mesothelioma advances and you have fewer options.
Mesothelioma pericardial effusions are classified based on their fluid source and appearance. For example, a malignant effusion occurs in those with mesothelioma. Each category potentially shifts treatment options. Some are more lethal than others.
Kinds of Pericardial Effusions
Doctors analyze the mesothelioma pericardial effusion fluid to assess the type. This analysis is crucial and dictates the next steps.
Sometimes, there is no definitive cause or reason for mesothelioma pericardial effusion. This makes it imperative to analyze risk factors and treat the underlying diseases. Regular medical check-ups are essential for continued assessment.
Causes of Pericardial Effusion
Registered nurse and mesothelioma expert Sean Marchese, MS, RN, tells us that prevention isn’t always possible. He says, “Pericardial effusion is often not something we can completely prevent, especially with certain cancers like mesothelioma. The good news is that doctors are always monitoring you for it, and there are very effective ways to manage it if it does happen.”
The rarest form of mesothelioma is the pericardial variety. These tumors create inflammation inside the heart sac, causing too much fluid around the heart. Its location can make it challenging to diagnose early. Modern Pathology reports that fewer than 1% of mesothelioma patients have this type, which affects 10 to 15 people in the U.S. every year.
Many people are only diagnosed once symptoms set in. This delay is why early diagnosis and treatment are so valuable to ensure effectiveness. Doctors use imaging to detect changes that could lead to mesothelioma pericardial effusion. Acting fast can mean the difference between a swift recovery and a dangerous complication.
It’s not unusual to diagnose pericardial mesothelioma as an incidental finding. You’re going to treat pericardial effusion. You’re not suspecting mesothelioma. Pericardial mesothelioma accounts for 1% to 2% of all mesothelioma, which is a rare disease.
Symptoms of mesothelioma pericardial effusion, such as shortness of breath, chest pain and fatigue, mirror heart and lung issues. These symptoms aren’t definitive, with many people experiencing various symptoms at the same time. However, the European Society of Cardiology notes nearly 90% of patients with pericardial effusion experience chest pain.
Common Pericardial Effusion Symptoms
When excess fluid develops, it creates pressure on the heart, and with more pressure, symptoms increase in severity. Many people don’t notice anything wrong at first. Symptom development can occur gradually or immediately. This variance is why early detection through imaging is key.
The most severe complication is cardiac tamponade. Cardiac tamponade occurs when pressure on the heart becomes too much, and the heart can’t pump effectively, necessitating emergency drainage of the fluid.
Complications of Pericardial Effusion
These complications can be deadly. Understanding your symptoms reduces your risk of complications associated with mesothelioma pericardial effusions.
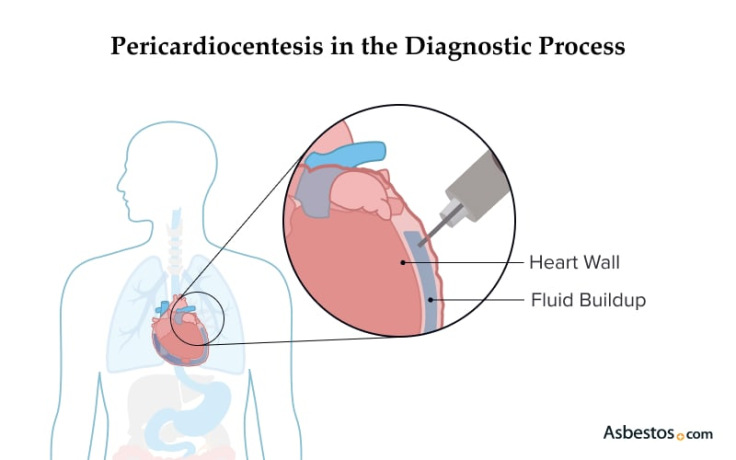
Doctors use core diagnostic tools that include physical exam, medical history and imaging such as CT scans and echocardiogram. Fluid can also be drained in a procedure called pericardiocentesis.
Pericardiocentesis involves inserting a needle to drain excess fluid for testing and to relieve pressure. The fluid is collected and analyzed to help determine the diagnosis and cause of the pericardial effusion.
Treatment depends on the amount of fluid and the strain it places on your cardiac function. If the effusions recur, your doctor will treat the cause of pericardial effusion directly, such as cancer or viral infections.
Pericardial Effusion Treatments
These measures reduce pressure on the heart and the risk of complications. Doctors will also follow up with you to ensure the fluid level is within normal limits. Adjustments in treatment may be indicated if levels change.
Patients with pericardial effusion from mesothelioma require multiple specialists. Oncologists and cardiologists collaborate for the best solution. Since no two patients are the same, tailored treatment is always better for patient outcomes.
People with pericardial effusions from mesothelioma require more aggressive treatment options such as pericardiectomy. This mesothelioma surgery is recommended because it can remove the tumor mass and avoid the possibility of fluid reaccumulation. Chemo or radiation can further reduce any tumors.

Connect with top-rated doctors specializing in mesothelioma treatment, who will personalize treatment options based on your diagnosis.
Find Your DoctorMany people with pericardial mesothelioma live with pericardial effusion as long as it doesn’t compromise their cardiac function. For people whose pericardial effusion becomes malignant, the outlook is less favorable.
A study published in the International Heart Journal in January 2024 tracked 171 patients with pericardial effusion for 2.5 years. A total of 21 patients, about 12.35%, passed away during follow-up. Additionally, 24 patients, or 14%, had to be hospitalized.
The study showed the survival rate is higher when intervention occurs sooner with targeted drainage and treatment. The key is early detection and treatment.
Follow up with your physician for proper maintenance to avoid repeated episodes. Support from Patient Advocates is available for patients and families.
Chest pain, shortness of breath and dizziness, also known as syncope, should receive emergency care. These symptoms suggest cardiovascular compromise, which can be treated early to avoid complications later. Inform your doctor if you have a history of cancer.
Anything greater than 500 milliliters, approximately more than 2 cups of liquid, constitutes a large pericardial effusion. This amount can compress the heart and require immediate intervention. Imaging can determine the amount.
Yes, especially in people with cancer. If the cancer isn’t well-managed, it may require repeat drainage or surgery. With follow-up care, the condition can be managed over time.
An untreated mesothelioma pericardial effusion can lead to heart failure as well as cardiac tamponade. Excess fluid build-up can cause damage to the heart over time. These complications can be prevented with screening and early intervention.
Stay up-to-date on treatment, research, clinical trials, doctors and survivors
The information on this website is proprietary and protected. It is not a substitute for professional medical advice, diagnosis or treatment. Any unauthorized or illegal use, copying or dissemination will be prosecuted. Please read our privacy policy and terms of service for more information about our website.
This website and its content may be deemed attorney advertising. Prior results do not predict a similar outcome.
The Mesothelioma Center’s claim as the most trusted resource is based on our more than 150 5-star Google and BBB reviews. Our organization also helps more than half of all mesothelioma patients annually diagnosed.
Your web browser is no longer supported by Microsoft. Update your browser for more security, speed and compatibility.
If you are looking for mesothelioma support, please contact our Patient Advocates at (855) 404-4592
The Mesothelioma Center at Asbestos.com has provided patients and their loved ones the most updated and reliable information on mesothelioma and asbestos exposure since 2006.
Our team of Patient Advocates includes a medical doctor, a registered nurse, health services administrators, veterans, VA-accredited Claims Agents, an oncology patient navigator and hospice care expert. Their combined expertise means we help any mesothelioma patient or loved one through every step of their cancer journey.
More than 30 contributors, including mesothelioma doctors, survivors, health care professionals and other experts, have peer-reviewed our website and written unique research-driven articles to ensure you get the highest-quality medical and health information.
My family has only the highest compliment for the assistance and support that we received from The Mesothelioma Center. This is a staff of compassionate and knowledgeable individuals who respect what your family is experiencing and who go the extra mile to make an unfortunate diagnosis less stressful. Information and assistance were provided by The Mesothelioma Center at no cost to our family.LashawnMesothelioma patient’s daughter


Asbestos.com. (2026, February 13). Pericardial Effusion. Retrieved February 26, 2026, from https://www.asbestos.com/mesothelioma/pericardial/effusion/
"Pericardial Effusion." Asbestos.com, 13 Feb 2026, https://www.asbestos.com/mesothelioma/pericardial/effusion/.
Asbestos.com. "Pericardial Effusion." Last modified February 13, 2026. https://www.asbestos.com/mesothelioma/pericardial/effusion/.

Dr. Velotta is a leading thoracic surgeon and pleural mesothelioma specialist at Kaiser Permanente Oakland Medical Center and a Clinical Assistant Surgical Professor at the University of California, San Francisco School of Medicine. With more than 15 years of experience, he leads research efforts in minimally invasive lung cancer surgery, pain management post-thoracic surgery and multimodal mesothelioma treatment. He is recognized for advancing image-guided surgical techniques and improving regional access to specialized mesothelioma care.
Our fact-checking process begins with a thorough review of all sources to ensure they are high quality. Then we cross-check the facts with original medical or scientific reports published by those sources, or we validate the facts with reputable news organizations, medical and scientific experts and other health experts. Each page includes all sources for full transparency.
Please read our editorial guidelines to learn more about our content creation and review process.
