
Hear from one of the nation’s top thoracic surgeons about how surgery can be effective for certain people with pleural mesothelioma.
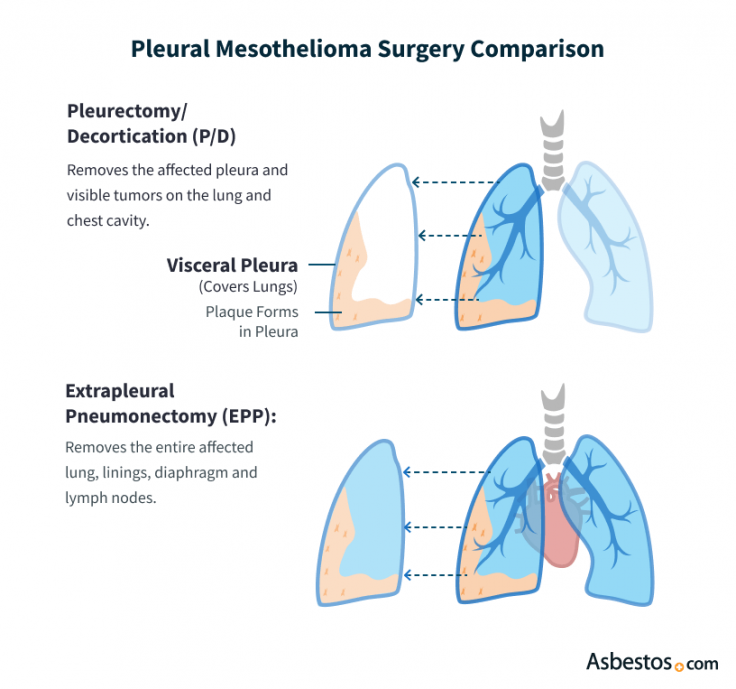
Reserve Your SpotPleurectomy/decortication (P/D) and extrapleural pneumonectomy (EPP) are the two most common tumor-removing surgeries for pleural mesothelioma. P/D is associated with fewer complications and better quality of life, but surgeons may choose an EPP if cancer has spread into the lung.
The goal of pleurectomy/decortication (P/D) and extrapleural pneumonectomy (EPP) is to remove all pleural mesothelioma cancer growth, relieve symptoms and extend the patient’s life span. Because both surgeries are performed locally in the chest cavity, they work best when the cancer has been found as early as possible and not spread outside of the chest cavity.
If the mesothelioma has advanced to a late stage and is no longer localized, neither procedure may provide significant benefit for the patient. In addition, a patient must be in good overall health to survive and recover from any major chest surgery. Otherwise, it cannot safely be offered even in early-stage cases.
P/D may involve scraping cancer cells off the surface of a lung, but it leaves both lungs intact. Most thoracic surgeons now prefer the P/D procedure for this reason, but they will still perform an EPP if they determine it is the only way to remove as much tumor growth as possible.

Hear from one of the nation’s top thoracic surgeons about how surgery can be effective for certain people with pleural mesothelioma.
Reserve Your SpotBoth P/D and EPP improve survival rates for pleural mesothelioma patients, especially when combined with other treatments as part of multimodal therapy. In a 2022 study, mesothelioma patients who underwent EPP had a median overall survival of 15 months versus 22 months for those who underwent pleurectomy and decortication surgery.
Some studies have associated P/D with longer survival times than EPP, but this does not necessarily mean the survival advantage comes from the procedure. Many factors are associated with survival including the cancer stage and indications to select one procedure versus the other.
The cancer stage and cell type, the patient’s age and the types of adjuvant therapies used all affect survival times much more than the type of surgery performed.
When choosing between EPP and P/D, the surgeon will consider the patient’s specific medical needs and preferences. Many thoracic surgeons are more comfortable with one procedure than the other, so the patient’s choice of cancer center and mesothelioma specialist may influence the type of surgery they receive.
| Pleurectomy/Decortication (P/D) | Extrapleural Pneumonectomy (EPP) |
|---|---|
| Less invasive: Removes the lining of the lung and other nearby tissues, but leaves lung intact | More invasive: Removes the lung and surrounding tissues, reducing patient’s quality of life |
| Lower mortality rate: 1–2% of patients die during or immediately after surgery | Higher mortality rate: 4–5% of patients die during or immediately after surgery |
| Less severe complications: May cause prolonged air leak in chest | More severe complications: May cause abnormal heart rate or arterial blockage |
If the patient is a candidate for surgery, the surgeon will consider the size and location of the tumor. If the tumor is localized to the pleural lining, P/D may suffice, but if the tumor has spread to the lung, EPP may be necessary to remove a greater portion of the tumor.
Mesothelioma specialists can use a variety of imaging scans to try to assess the extent of the cancer’s spread, but in many cases, a surgeon will not make the final judgment call until they have opened the patient’s chest cavity during surgery and seen the extent of the tumor growth directly. A surgeon may begin surgery intending to perform P/D but then realize an EPP would be better, or the other way around.
We’re finding that we’re able to remove all the tumor that’s visible even with the lung-sparing pleurectomy/decortication. That is why there has been a shift toward doing [P/D] more so than in decades past.
Choosing between the two procedures is complex, but both surgeries can give the patient a good chance to live longer with pleural mesothelioma. A mesothelioma specialist is the best doctor to help a patient and their loves ones make the decision between an EPP or the P/D surgeries.
Recommended ReadingStay up-to-date on treatment, research, clinical trials, doctors and survivors
The information on this website is proprietary and protected. It is not a substitute for professional medical advice, diagnosis or treatment. Any unauthorized or illegal use, copying or dissemination will be prosecuted. Please read our privacy policy and terms of service for more information about our website.
This website and its content may be deemed attorney advertising. Prior results do not predict a similar outcome.
The Mesothelioma Center’s claim as the most trusted resource is based on our more than 150 5-star Google and BBB reviews. Our organization also helps more than half of all mesothelioma patients annually diagnosed.
Your web browser is no longer supported by Microsoft. Update your browser for more security, speed and compatibility.
If you are looking for mesothelioma support, please contact our Patient Advocates at (855) 404-4592
The Mesothelioma Center at Asbestos.com has provided patients and their loved ones the most updated and reliable information on mesothelioma and asbestos exposure since 2006.
Our team of Patient Advocates includes a medical doctor, a registered nurse, health services administrators, veterans, VA-accredited Claims Agents, an oncology patient navigator and hospice care expert. Their combined expertise means we help any mesothelioma patient or loved one through every step of their cancer journey.
More than 30 contributors, including mesothelioma doctors, survivors, health care professionals and other experts, have peer-reviewed our website and written unique research-driven articles to ensure you get the highest-quality medical and health information.
My family has only the highest compliment for the assistance and support that we received from The Mesothelioma Center. This is a staff of compassionate and knowledgeable individuals who respect what your family is experiencing and who go the extra mile to make an unfortunate diagnosis less stressful. Information and assistance were provided by The Mesothelioma Center at no cost to our family.LashawnMesothelioma patient’s daughter


Selby, K. (2026, February 18). Pleurectomy Decortication (P/D) vs. Extrapleural Pneumonectomy (EPP). Asbestos.com. Retrieved February 20, 2026, from https://www.asbestos.com/treatment/surgery/pleurectomy-vs-pneumonectomy/
Selby, Karen. "Pleurectomy Decortication (P/D) vs. Extrapleural Pneumonectomy (EPP)." Asbestos.com, 18 Feb 2026, https://www.asbestos.com/treatment/surgery/pleurectomy-vs-pneumonectomy/.
Selby, Karen. "Pleurectomy Decortication (P/D) vs. Extrapleural Pneumonectomy (EPP)." Asbestos.com. Last modified February 18, 2026. https://www.asbestos.com/treatment/surgery/pleurectomy-vs-pneumonectomy/.

Dr. Landau is the Medical Director of Virtual Hematology at the Medical University of South Carolina, where he leads programs that expand access to cancer care through telehealth. With more than 18 years of experience in oncology and hematology, he specializes in hematologic and genitourinary cancers, including bladder, prostate and kidney cancers. He has held multiple leadership roles in cancer program development and previously served as section chief of hematology and oncology at Orlando Health UF Health Cancer Center, where he founded its telehealth program.
Our fact-checking process begins with a thorough review of all sources to ensure they are high quality. Then we cross-check the facts with original medical or scientific reports published by those sources, or we validate the facts with reputable news organizations, medical and scientific experts and other health experts. Each page includes all sources for full transparency.
Please read our editorial guidelines to learn more about our content creation and review process.
