p53 Gene Therapy
The p53 tumor-suppressor gene helps the body fight cancer cells. Mutations in this gene are associated with all types of cancer. Gene therapy to fix or replace defective p53 genes is a new way to treat cancers such as mesothelioma.
What Is p53 Gene Therapy?
The p53 gene therapy is an innovative cancer treatment strategy. It involves repairing or replacing a gene that produces the tumor-suppressor protein p53. The p53 protein is often called the “guardian of the genome.” It repairs DNA and prevents uncontrolled cell growth and cancer.
Restoring the body’s ability to produce functioning p53 protein is the goal of p53 gene therapy. Mutations in this gene appear in more than 50% of all cancers. But they are rarely seen in healthy tissue. Targeting p53 may help treat and possibly cure mesothelioma and other cancers.
Therapies to Treat p53 Mutations
- Degrading or inactivating mutated p53 protein
- Inducing cell death in cells with dangerous p53 mutations
- Reactivating the p53 gene to produce functioning p53
- Restoring or stabilizing the normal shape of the p53 protein
Many experts believe p53 gene therapy can treat various cancers, including mesothelioma. Several interventions target p53 mutations. They include gene therapy and drugs that restore or inactivate p53. The drugs aim to fix the mutated p53 genes and proteins.
Different mutations are susceptible to different treatments. Some treatments only work when specific mutations are present. Sometimes, p53 gene mutations cause defective p53 protein to build up in cells. This can lead to cancer. Some treatments aim to degrade these defective proteins.
How Does p53 Gene Therapy Work?
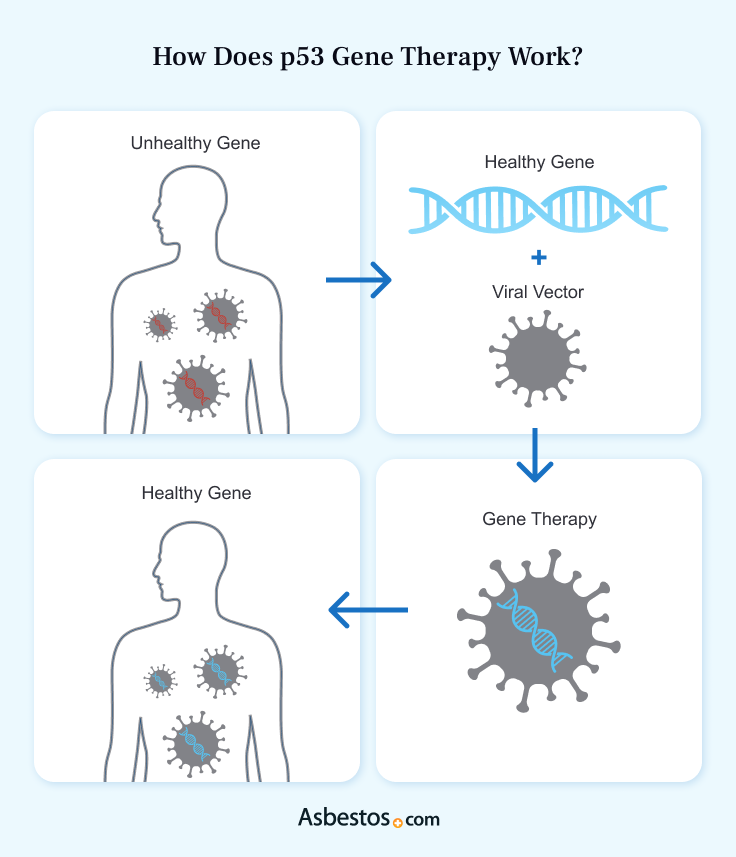
Gene therapy inserts a functioning gene into cells with a mutated gene. The cell’s DNA takes in this gene, allowing it to produce a working protein. The U.S. Food and Drug Administration hasn’t approved many gene therapies. This treatment may be available in clinical trials.
Doctors can safely combine p53 gene therapy with other cancer treatments. For example, doctors may use radiation, chemotherapy, immunotherapy and surgery combos. This may increase your treatment’s effectiveness.
Another form of gene therapy in development for mesothelioma includes suicide gene therapy. Doctors are trying to figure out how to fix or replace damaged p53 genes in cancer cells. It could help treat different types of cancer.
Challenges of Delivering the p53 Gene
The biggest challenge of gene therapy is getting working genes into cells with faulty ones. Successful treatment requires delivering genes to the right cells. Then, the cells’ DNA must incorporate the genes. There are several methods to achieve this, including using viruses and nanoparticles.
Ongoing trials are testing p53 gene therapy for mesothelioma treatment. For example, researchers are testing it in combination with other treatments.
Nonreplicating Vectors
Genetically engineered viruses can deliver gene therapy to cells. Researchers use several types of viruses as vectors to transfer DNA into human cells. Scientists change these viruses to prevent them from replicating or causing infections.
Doctors can inject these altered viruses into the body, sometimes directly into tumors. This method of delivering gene therapy has proven safe and effective. But it isn’t efficient. These viruses may not reach all cancer cells. The immune system may destroy them before they reach their target.
Oncolytic Viruses
Oncolytic viruses are genetically altered viruses. They attack cancer cells and spare healthy ones. These viruses can also serve as vectors to carry DNA to cancer cells. Research shows oncolytic viruses can transfer p53 genes to cancer cells. This increases their ability to destroy the cancer cells.
Researchers have used a modified variation of the measles virus to fight mesothelioma. Laboratory studies show oncolytic viral therapy may treat mesothelioma effectively. This is true with or without gene therapy.
Nanoparticles
Nanoparticles can transfer DNA or other molecules into cells. They’re no larger than 100 nanometers. That’s 1,000 times smaller than a human hair’s thickness.
These nanoparticles are more efficient than viruses for delivering gene therapy to cancer cells. Scientists can design nanoparticles to target only cancer cells. Research suggests nanoparticles may safely restore p53 function in cancer cells.
Reactivating p53 with Drugs
Some new and existing drugs affect the p53 gene or protein. There are many possible mutations in the p53 gene. Some prevent cells from making p53 protein. Others cause abnormal p53.
Drugs that let cells make a working p53 protein can treat some mutations. These mutations block cells from making this protein. Other drugs can stabilize the p53 protein’s 3-D shape. This shape is vital for the protein to work properly. Several drugs are in trials to test their ability to treat cancer.

Try our new clinical trials search tool to find active trials near you. Get help enrolling today.
Find a Clinical TrialBenefits of p53 Gene Therapy
A major benefit of p53 gene therapy is that it can target cancer cells. Other treatments that target p53 can do the same. Cancer drugs can harm healthy cells as well as cancer cells. This causes many side effects. Targeting only cancer cells or cells with p53 mutations may reduce side effects.
Studies show p53 gene therapy can reverse cancer cells’ resistance to radiation. It can also lessen radiation’s side effects. p53 gene therapy works best with other cancer treatments. Examples include radiation, immunotherapy or chemotherapy.
Adding p53 to some tumor cells or activating WT p53 in tumor cells can result in cell death, tumor remission or even cures.
Research shows this therapy is safe and effective for certain cancers with p53 mutations. For example, researchers have tested Gendicine in trials on several cancers. Gendicine is a viral vector containing the p53 gene.
Tests of other p53-based treatments in cells and animals were successful. Researchers will need to conduct human trials as well.
Side Effects of p53 Gene Therapy
The side effects of p53 gene therapy are typically mild compared to those of chemotherapy or radiation. The most common side effect is flu-like symptoms. They include fever and pain after taking the drug. Gastrointestinal symptoms are also common.
Most reactions to p53 gene therapy are mild. However, serious side effects can occur. These include kidney and liver dysfunction and bone marrow suppression. A rare and serious side effect is platelet crisis. This can cause spontaneous bleeding. It’s a life-threatening condition.
Possible Adverse Reactions to P53 Gene Therapy
- Decreased blood cell production (bone marrow suppression)
- Fever
- Flu-like symptoms
- Gastrointestinal symptoms
- Liver dysfunction
- Muscle or joint pain
- Pain at the injection site
- Red blood cells breaking down (hemolysis)
Some side effects seen in clinical trials depend on the location of the cancer. For example, treatment can harm the lungs of lung cancer patients. It can also cause urinary problems in cervical cancer patients.
Find the top cancer centers trusted by mesothelioma patients nationwide.
Get Help Nowp53 Gene Therapy Clinical Trials
Clinical trials are vital. They test new treatments to ensure they’re safe and effective. There is no FDA-approved gene therapy for mesothelioma. The only way to access this treatment is in a clinical trial. Clinical trials for p53 gene therapy and p53-based treatments are ongoing around the country.
Recruiting Clinical Trials
- The Evaluation of PC14586 in Patients With Advanced Solid Tumors Harboring a TP53 Y220C Mutation (PYNNACLE)
- JAB-30355 in Patients With Advanced Solid Tumors Harboring TP53 Y220C Mutation
There are clinical trials for drugs that interact with p53 and MDM2, which regulates p53. Your mesothelioma doctor and Asbestos.com Patient Advocates can help. They can provide info on clinical trials you may qualify for.
Can p53 Gene Therapy Be Used to Treat Mesothelioma?
Research shows p53 gene therapy may be able to treat certain mesothelioma cases. However, only people with p53 mutations can benefit from p53 gene therapy.
A 2022 research study found p53 mutations in 18% of pleural mesothelioma and 15% of peritoneal mesothelioma cases. This means more than 80% of mesothelioma patients have a functioning wild-type p53 gene. So they may not benefit from this treatment.
Lab research has paved the way for clinical trials. They’ll test p53-based treatments for mesothelioma. Cell cultures show p53 gene therapy can boost chemo for pleural mesothelioma.
Soon, new mesothelioma treatments that target p53 may be in clinical trials. Treatments focusing on p53 and its role in tumor growth may change how we treat mesothelioma and other cancers.
Recommended Reading


