Pericardial Effusion
Pericardial effusion is the main symptom of pericardial mesothelioma. The fluid buildup seen in pericardial effusion can also be caused by infections, inflammation and other cancers. The fluid buildup puts pressure on the heart and may lead to heart failure.
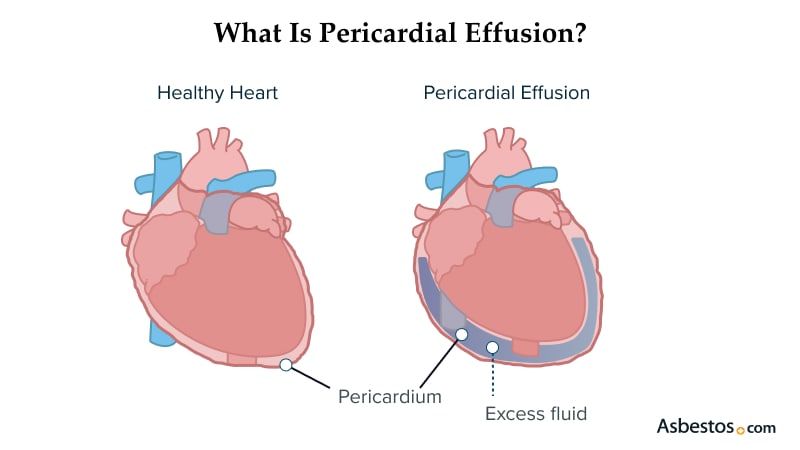
What Is Pericardial Effusion?
Pericardial effusion is the buildup of excess fluid between the tissues that line the heart. This lining, called the pericardium, has two layers. A small amount of fluid between these layers lubricates and protects the heart. Extra fluid in pericardial effusion puts added pressure on the heart and results in damage.
Pericardial effusion can develop from mesothelioma, other cancers, infections and chest injuries. If you have symptoms of pericardial effusion, talk to your doctor. They will drain the fluid to relieve your symptoms and determine the cause.
What Causes Pericardial Effusion?
Pericardial effusions are caused by mesothelioma, radiation therapy and infection. They cause inflammation and trigger fluid buildup.
Causes of Pericardial Effusion
- Bacterial, viral, fungal or parasitic infections
- Cancer, including mesothelioma and lung cancer
- Certain chemotherapy drugs such as doxorubicin and cyclophosphamide
- Inflammation, including inflammation of the heart lining
- Pleural mesothelioma or other cancers of the chest
- Radiation therapy to the chest
- Traumatic injuries to the heart
- Underactive thyroid
In most cases, doctors do not know the cause of pericardial effusion. This is known as an idiopathic pericardial effusion.
Types of Pericardial Effusion
There are several types of pericardial effusion based on the cause. Doctors also divide effusions into exudative and transudative. This depends on the substances in the fluid.
Pericardial Effusion Types
- Cardiac: Develops as a result of a heart attack or heart surgery
- Idiopathic: Has no known cause
- Infectious: Develops from infections with a variety of pathogens
- Inflammatory: Develops from autoimmune disorders that cause body-wide inflammation, such as rheumatoid arthritis or systemic lupus erythematosus
- Neoplastic: Caused by tumors in the chest or around the heart. These can be primary or metastatic.
- Traumatic: Forms from injuries to the heart or its vessels that let fluid accumulate around the heart.
- Vascular: Caused by tears in the aorta
Transudative pericardial effusions are liked with heart failure, hypoalbuminemia, post-radiation therapy and renal insufficiency. Exudative effusions follow pericardial inflammation, infections and malignant or auto-immune events.
Mesothelioma and Pericardial Effusion
Mesothelioma can cause pericardial effusion if it develops in the pericardium. Pericardial mesothelioma is rare, and it’s associated with a poor prognosis or outlook.
If you’ve been exposed to asbestos, your doctor may link your pericardial effusion to mesothelioma. Pericardial effusion may be one of the first signs of pericardial mesothelioma.
It’s not unusual to diagnose pericardial mesothelioma as an incidental finding. You’re going to treat pericardial effusion. You’re not suspecting mesothelioma. Pericardial mesothelioma accounts for 1% to 2% of all mesothelioma, which is a rare disease.
What Are the Symptoms of Pericardial Effusions?
The most common symptoms of pericardial effusion are shortness of breath and chest pain. The extra fluid presses on the heart, making it harder for it to pump blood effectively.
Common Pericardial Effusion Symptoms
- Chest pain
- Fatigue
- Edema or swelling in the legs and feet
- Shortness of breath that worsens when you lie down and improves when you sit up
Pericardial effusion can become dangerous if left untreated. Many of the symptoms of pericardial effusion also mimic other heart and lung conditions. If you are experiencing any of these symptoms, you should talk to your doctor.

Understand your diagnosis, top doctors and ways to afford care.
Get Your Free GuidePericardial Effusion Diagnosis
Pericardial effusions are diagnosed using an echocardiogram and pericardiocentesis. The preferred test for diagnosing pericardial effusion is an echocardiogram. It can be either transthoracic or transesophageal. These methods use ultrasound waves to image the heart and fluid buildup.
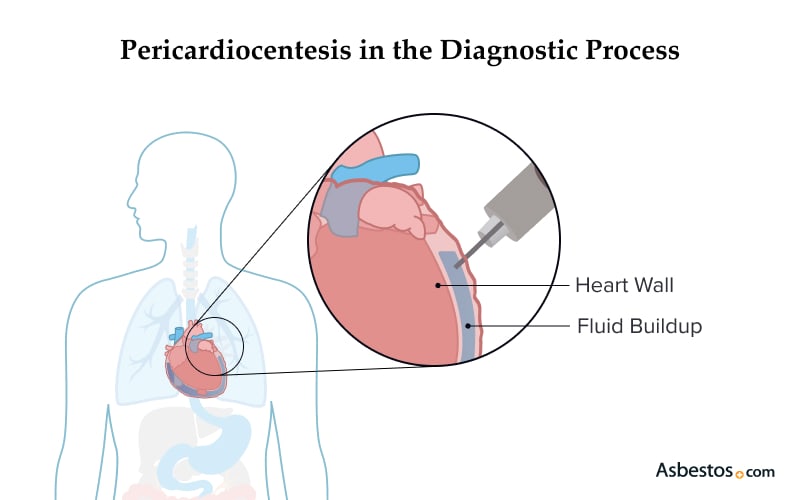
Your doctor may order a pericardiocentesis to find the cause of the pericardial effusion. This procedure drains fluid around the heart. A lab analyzes the fluid to check for infection, cancer, inflammation or other causes of the effusion.
Pericardial Effusion Treatment
Treatment for pericardial effusion depends on its cause, your symptoms and health. If the effusion is small and does not affect heart function, the doctor will observe it over time. They may order additional imaging tests to check the effusion and confirm if it is not growing larger.
Medications treat the cause of pericardial effusion. Doctors use antibiotic therapy to treat bacterial infections. Anti-inflammatory drugs also help prevent complications such as cardiac tamponade.
Severe pericardial effusions causing symptoms or preventing the heart from pumping effectively need to be drained. There are two methods to treat pericardial effusions.
Pericardiocentesis
Pericardiocentesis is a procedure that removes excess fluid surrounding the heart muscle. Doctors use this approach to diagnose and treat a pericardial effusion.
Steps of a Pericardiocentesis
- The doctor numbs an area of the chest.
- They prepare the skin and use an ultrasound to find the infusion’s location.
- The doctor inserts a needle into the chest and guides it to the heart, then removes the fluid.
- The removed fluid is sent to a lab for analysis. This will determine the cause of the pericardial effusion.
Pericardiocentesis is effective for treating pericardial effusions. They are also simple to perform and can be done at the bedside in the hospital. However, it is possible the effusion returns after pericardiocentesis.
Pericardiectomy
A pericardiectomy is surgery to remove the pericardium from around the heart. Doctors may remove only the affected part of the pericardium. This is called a partial pericardiectomy. A total pericardiectomy removes as much of the pericardium as possible.
The pericardiectomy procedure is more intensive than pericardiocentesis, but it is less likely that the effusion will return. Your doctor will weigh the pros and cons of each procedure with you to determine which is best. They will check your health and your ability to tolerate open-heart surgery with pericardiectomy.
Complications of Pericardial Effusion
Most cases of pericardial effusion have few complications. However, an effusion can lead to severe health issues.
Possible Pericardial Effusion Complications
- Cardiac tamponade: Excess fluid compresses the heart, preventing it from pumping blood.
- Constrictive-effusive pericarditis: The loss of the heart muscle’s elasticity, making it harder to fill with blood.
- Pericardial empyema: A collection of pus in addition to the fluid surrounding the heart due to infection.
The more severe the pericardial effusion, the more likely it is to develop a complication. If these complications appear, you should contact your doctor as soon as possible.
Living With Pericardial Effusion
If you have pericardial effusion, you may wonder about your prognosis. A 2024 study published in the International Heart Journal tracked 171 patients with pericardial effusion for 2.5 years. In total, 21 patients (12.35%) died during follow-up. Also, 24 patients (14%) were hospitalized.
Your prognosis with pericardial effusion depends mainly on its cause. The same study of 171 patients found that cancer was the leading cause of death in those with pericardial effusion. Patients treated with radiation and those with cancer were more likely to develop heart conditions.
Can Pericardial Effusion Be Prevented?
Pericardial effusion is hard to predict. So, it may not be possible to prevent it. You can take extra steps to support your heart health and reduce complications. Doctors recommend quitting smoking and eating a heart-healthy diet.
Pericardial effusion from mesothelioma is hard to predict. Mesothelioma is a slow-growing cancer. It develops 20 to 60 years after asbestos exposure. Many people were not aware of their exposure at the time it happened. If you have a history of asbestos exposure, you are eligible for mesothelioma screening. This includes exposure from your job or a family member.
Common Questions About Pericardial Effusions
- What is the most common cause of pericardial effusion?
-
The most common cause of pericardial effusion is lung cancer. Other causes include pericardial mesothelioma, infections, chest injuries, and radiation therapy.
- When should I see a doctor for my symptoms?
-
Pericardial effusion is a serious condition, and you should see your doctor as soon as possible. You will need treatment to remove the extra fluid around your heart to prevent long-term damage.




