The Caregiver Shortage: Which States Are Doing Best?
Written by Sean Marchese, MS, RN | Edited By Walter Pacheco
The Growing Caregiver Shortage
Caregivers working as personal care aides, home health aides and nursing assistants provide services for older adults, people living with physical, intellectual or developmental disabilities and people living with chronic illnesses such as lung cancer or dementia.
As the American population continues to age, the country struggles to keep up with the growing demand for paid caregivers. And, according to one AARP report, three out of four seniors over 50 want to age in place at home. Those same older adults will need additional assistance, typically from paid or family caregivers, to thrive at home.
The Statistics Behind the Caregiver Shortage
Caregivers provide a variety of vital services for millions of older adults in the United States.
- 20 million seniors and people with disabilities require long-term services and support. And most want them at home or in the community, as opposed to in an institution.
- Approximately 800,000 older Americans needing subsidized care are on waiting lists because of the lack of available workers.
- Direct support professionals working with adults with intellectual and developmental disabilities had an average national turnover rate of 43% in 2019.
To assist in visualizing the overall American caregiver shortage, we have gathered the most recent statistics on the employment, salary, job growth and future job potential for direct service caregivers in each state.
How does your state compare?
Caregiver Job Stats by State
Click on a state to reveal the statistics or use the dropdown menu below.
How the States Stack Up in the Caregiver Shortage
The impact of the shortage can be seen across every state. California employs the most caregivers, while Alaska features the highest average hourly wage for its caregivers.
The Best States for Caregivers
It may come as no surprise that New York is the top performer when it comes to the caregiver workforce. It is home to the best ratio of caregivers, with almost 30 available for every 1,000 state residents. It ranks second for both the average wage at $17.49 an hour and the projected number of caregiver jobs by 2028.
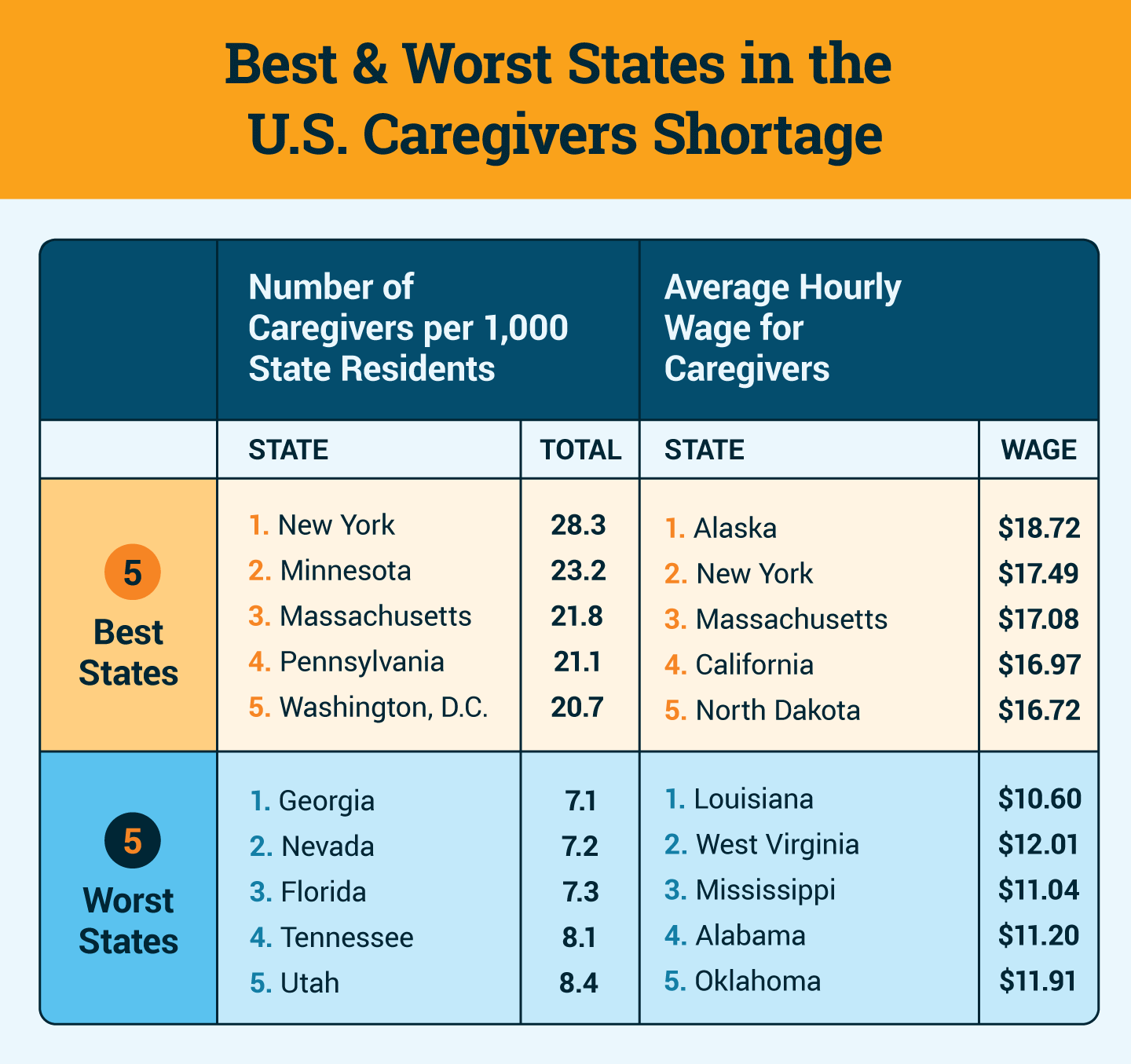
California is the state with the most opportunities for caregivers. The Golden State saw a caregiver job growth rate of 231% between 2010 and 2020, more than two times the rate of Massachusetts, which came in second place. Aspiring caregivers can look to California, too, as more than 1.2 million jobs are projected to be available by 2028. That’s over 130,000 more job openings than New York, which ranked second in this category.
Overall, Massachusetts was also a strong performer. In addition to coming in second in job growth over the past decade, the state offers the third-best hourly pay ($17.08) and the third-highest ratio of caregivers to state residents, at 21.8 caregivers for every 1,000 people.
The States Where Caregivers Are Struggling
Our review of these national datasets revealed that several states are struggling to meet the needs of caregivers. As a result, fewer direct care workers enter the workforce in these areas, thus impacting the people they serve. Specifically:
- Two Southern states were among the lowest-performing states.
- Louisiana provides an average hourly rate of $10.60, the lowest pay in all 50 states for caregivers. It also has one of the lowest projected 2028 job totals, at 10,500.
- Mississippi has the lowest projected future jobs total (2,200) and the second-lowest hourly wage in the country ($11.04).
- Vermont was the only state to experience a decrease in job growth over a 10-year period, dropping 5% in caregiver positions between 2010 and 2020.
Why Is There a Caregiver Shortage?
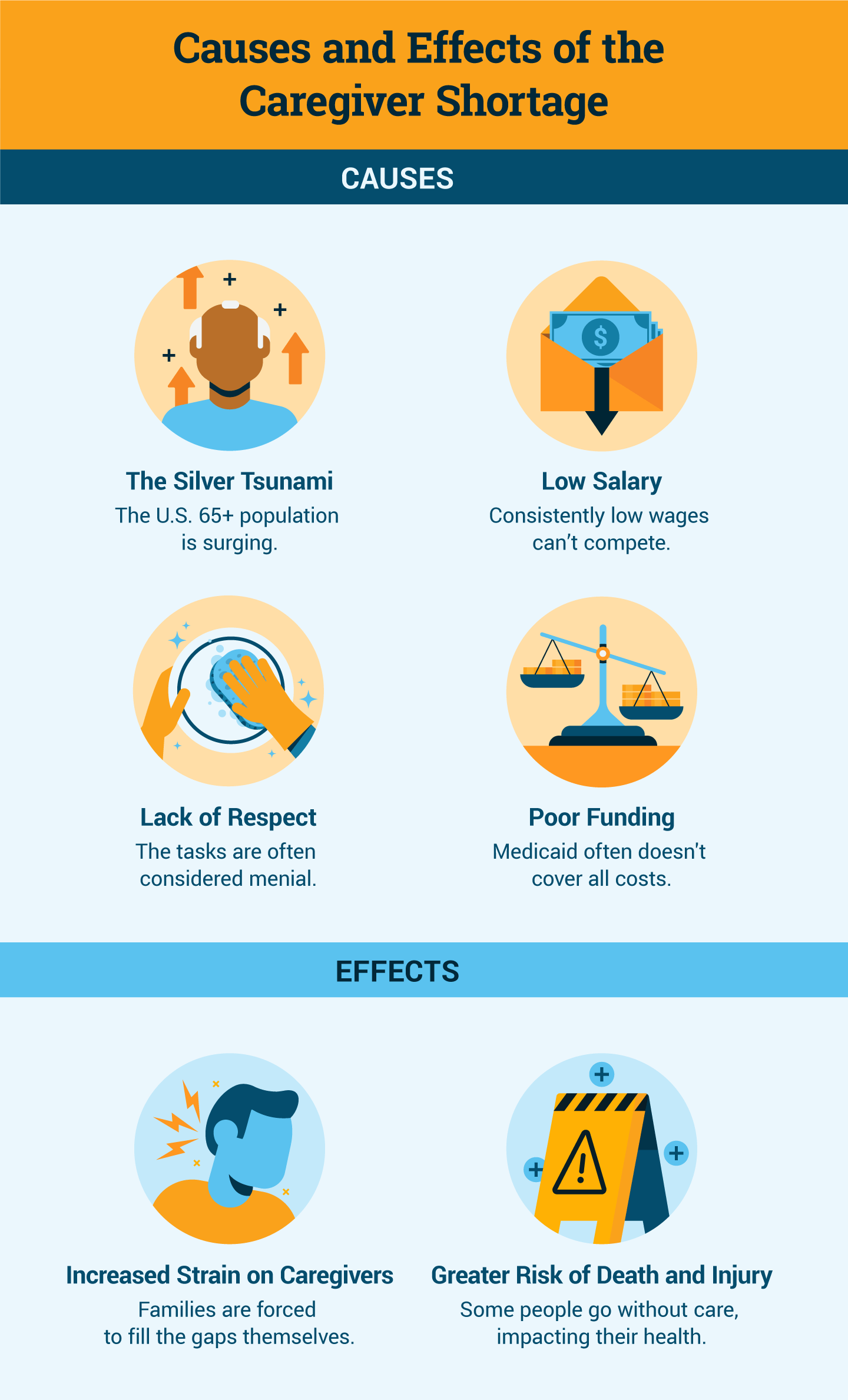
Steadily growing demand, consistently low pay and inadequate supply numbers have created the current caregiver shortage occurring across the country. A multitude of factors have led us to this point.
COVID-19 Made Things Worse
Concerns about caregiver numbers existed before COVID-19 forced the majority of the world’s population into lockdown. But the intensified strain the pandemic brought to every level of the health care system has worsened conditions for those who rely on caregivers for ongoing support.
Those aging in place at home during the pandemic faced challenges of isolation and missed care when caregivers could not enter their homes. Sadly, it became clear that those who were at home for the duration were in the safer setting, as more than 184,000 nursing home residents and staff died from COVID-19.
As a result of these many struggles, the American Network of Community Options and Resources reported in 2020 that 68% of all the direct support providers they surveyed had to close down one or more services due to the pandemic, resulting in an average loss of revenue of 32%. The survey respondents also overwhelmingly identified staffing as their No. 1 challenge, with 57% citing it as a major issue.
A Kaiser Family Foundation survey of Medicaid-funded home and community-based services for seniors and people living with disabilities found that two-thirds of responding states experienced at least one provider closing its doors permanently during the pandemic. Workforce shortages were cited as the most common reason for closures of in-home and group-home services.
The Silver Tsunami Is Increasing Demand
The United States is facing a larger population of adults over the age of 65 than ever before, primarily made up of baby boomers (those born between 1946 and 1964). This demographic group grew rapidly, exploding from 41 million people in 2011 to 71 million in 2019 — a massive 73% increase. The U.S. Census Bureau estimates this number will keep rising, projecting it will reach 82 million by 2030.
Seven out of 10 of these Americans aged 65+ will eventually need long-term care. Therefore, by 2030, the demand for home health care is anticipated to grow by 46% with more than 1 million new home care jobs needing to be filled.
Persistent Low Pay Adds to the Challenge
The median hourly wage for direct care workers in 2020 was $13.56. When comparing that to the federal minimum wage of $7.25, the career path looks promising. And most state minimum wages don’t surpass that pay rate either, except in Washington, California and the District of Columbia. But, in contrast, considering that fast-food chain McDonald’s has committed to raising its average minimum wage to $15 an hour by 2024, it provides perspective on the challenges of enticing new people into the direct care workforce.
A 2020 workforce equity study from Policy Link ranked home health aides as the fifth-lowest and personal care aides as the fourth-lowest-paying jobs among the 25 lowest-paying jobs disproportionately held by people of color. Only dishwashers, fast-food cooks and cafeteria attendants were paid less. Nursing assistants also made the list, ranking 19th.
Research has shown that low wages are often cited as the main reason 50% of direct care workers leave their jobs within the first year. They also point to strenuous workloads, lack of advancement opportunities and little to no health care benefits as additional issues leading them to quit.
A Disrespected Line of Work
Home health aides have pointed out they often feel disrespected by other medical workers and sometimes by their clients. Some have noted they are flatly ignored by nurses when providing updates on a client’s health. Clients may be dealing with intellectual delays that can cause them to lash out at the direct support worker trying to help them. Or they may simply be frustrated that they require assistance with daily tasks.
Lack of Funding to Help with Home Care
The need for the assistance of a direct support worker typically can last for many weeks and in some cases may last months or years based on the client’s health. The cost for such services quickly adds up. Government funding through Medicaid often helps cover some, but rarely all, of that expense, and families are asked to cover the bills. In addition, Medicare does not cover long-term home care at all.
Someone living with a disability may have been approved by state Medicaid for 40 hours of weekly care initially. Current caregiver shortages have recently caused that coverage to be reduced to only 20 hours a week due to the lack of available workers. Family members are faced with having their loved one forced into a nursing home if they cannot cover the remaining hours themselves.
Federal and state lawmakers across the country have spent years negotiating increases and cuts to home and community-based services for health care. Recently proposed expansions to Medicaid programs — in part to help raise the wages of home care workers — would cost hundreds of billions of dollars. If approved, some experts say it still won’t be enough to offset the severity of this shortage.
Ripple Effects of the Caregiver Shortage
Due to the sheer number of aging Americans, most people are likely to feel the effects of the caregiver shortage. The inability to rely on quality care — whether at home, in a nursing home or assisted living facility, or elsewhere — is bringing stress and strife to individuals and families across the country.
More Strain on Family Caregivers
According to a 2020 AARP report, 53 million Americans are currently unpaid caregivers. That’s one in five people providing care to an adult or child with special needs at some time in the last 12 months. The inherent stress of this task is highlighted by the 23% of family caregivers who say it’s made their own health worse.
With 61% of family caregivers also working, the juggling required to manage a loved one’s care takes a lot of energy and focus. Of those surveyed, 26% report having difficulty coordinating care in an effort to ease their burden.
Increased Risk of Medication Errors and Deaths
Potential health risks caused by the caregiver shortage include increased danger of falls, patients developing feelings of isolation, and physical deterioration if healthy eating and physical movement routines are disrupted.
When caregivers are not available, patients also experience more medication errors and mismanagement. Two out of five providers of community-based direct care services experienced an increase in reportable incidents as a direct result of insufficient staffing.
Important Factors in Solving the Caregiver Crisis
When looking at a complex problem like this, it’s obvious there is no simple solution. Strategies and practices must be closely examined and put into play. Legal policy revisions in several areas and digital innovation may spark needed changes.
Push to Broaden Scope-of-Practice Laws
Experts such as MIT Sloan School of Management professor Paul Osterman claim that changes to scope-of-practice laws in some states are necessary to give personal care aides the option to take on certain medical tasks after gaining additional training. Assuming duties such as light physical therapy, managing diabetes and Alzheimer’s care could reduce the workload of busy nurses on their client’s health care team.
Immigration Issues
Approximately one in four in-home caregivers is an immigrant. Changes in immigration laws and policies directly impact the workforce supply of people able and willing to take on these low-paying jobs. The caregiver labor pool would benefit from reformed immigration laws.
Developing New Technologies
New technologies like smartwatches and voice-activated devices hold the potential to benefit those in need of care and assist patients in communicating with their medical practitioners. Tech companies have taken note of this growing eldercare industry and are seeking ways to help.
Caregivers play a vital role in American health care, but this shortage is not an isolated occurrence. Nurses, physicians and other primary care professionals are experiencing documented shortages. Patient care, wait times and medical bills are also impacted.
The pandemic’s effect on the United States health care system focused a spotlight on many of these current shortages. By raising awareness of the challenges we face from the caregiver shortage and developing strategies to improve the situation, there is hope that the choice to pursue a career as a direct care worker will become more appealing and benefit us all.






