You shouldn’t have to choose between getting care and paying for it. Get the financial support you deserve.
Explore Your OptionsThe primary goal of curative treatment for asbestos-related lung cancer is to remove and kill cancer cells to prevent its spread. For patients in advanced stages of disease progression, treatment may focus on palliative care or reducing symptoms to improve quality of life.
Asbestos-related lung cancer treatment can involve various forms of surgery, chemotherapy and radiation. When you receive a lung cancer diagnosis, your doctor will explain what type of tumor you have. There are two main types of lung cancer: Small cell and non-small cell.
Small cell and non-small cell lung cancers grow, spread and react to treatments differently. When you receive your diagnosis, your doctor will also explain the stage your cancer is at in terms of its progression. Your specific cancer type will play an important role in determining the best treatment plan for you.
Exposure to asbestos is strongly associated with causing lung cancer, mesothelioma and several other severe respiratory diseases. Asbestos is the most common occupational risk factor for lung cancer, and workplace exposure significantly increases the chance of developing the disease.
The stage a patient’s cancer has progressed to may limit treatment options. Lung cancer can spread to the lymph nodes and distant organs as it progresses, making treatment increasingly difficult. The earlier the diagnosis, the more treatment options there are. This increases the likelihood of successful treatment.
Non-small cell lung cancers are commonly classified with a 4-stage system. A higher stage indicates more advanced disease.
Small cell lung cancer is staged using a 2-stage system: Limited stage or extensive stage. In limited stage, the cancer is only found in a single lung and possibly nearby lymph nodes. In extensive stage, the tumor has spread to both lungs or other organs.
Surgery’s goal is to remove a tumor and nearby cancerous tissue, ideally eliminating the disease completely. The tumor’s size, its location and how far the cancer has spread affects how much tissue is removed.
Types of surgery for lung cancer include: Wedge resection, lobectomy and pneumonectomy. Wedge describes the shape of the portion of lung and tissue removed in a wedge resection. A lobectomy removes a lobe, or section, of a lung. A pneumonectomy removes an entire lung.
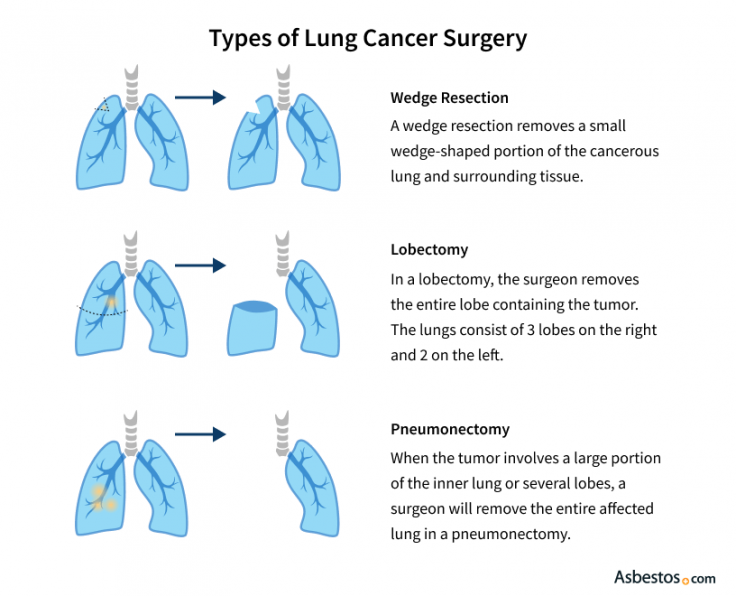
If the cancer is found in an early stage when spread is limited, curative surgery is preferred for its statistically high success rates. However, in advanced-stage cancer where a cure is unlikely, palliative surgery may be performed to relieve symptoms and make patients more comfortable.
In addition to a patient’s cancer stage, doctors look at the cancer’s type before recommending a curative surgery approach. Coexisting conditions, such as heart disease, could make a patient ineligible for surgery.
You shouldn’t have to choose between getting care and paying for it. Get the financial support you deserve.
Explore Your OptionsSurgery patients with non-small cell lung cancer can experience a 50-75% chance of relapse-free 5-year survival. In most cases, non-small cell lung cancers are removed through lobectomy. If the patient has poor lung function, however, doctors may remove only a small wedge of the lung via surgical resection.
Surgery is an option only in a few special cases of small cell lung cancer. This is because small cell lung cancer spreads much more aggressively than non-small cell lung cancer. Although surgical treatment for small cell is rare, studies have reported positive results for the small percentage of patients with very limited disease.
When there is clear evidence that lung cancer has spread from the initial tumor, chemotherapy is recommended. This treatment is typically not curative for lung cancer, but has been known to reduce the size of tumors and kill cancer cells that have spread to the lymph nodes. For patients, this usually translates to a longer, more comfortable life.
Whether taken intravenously or in pill form, chemotherapy drugs target rapidly dividing cells. This kills cancer cells, but can also affect normal healthy cells including hair follicles, red and white blood cells and the cells that line the stomach.
Because nearly 50% of all patients who have a tumor surgically removed will experience relapse, about 80% of all lung cancer patients are considered for chemotherapy during the course of their treatment.
More than 50%
The percentage of lung cancer patients who may experience a notable reduction in tumor size with modern chemotherapy, including use of targeted agents.
In the earliest stages of non-small cell lung cancer, chemotherapy is sometimes given before surgery to reduce tumor size and eliminate early spreading. Doctors call this approach neoadjuvant chemotherapy. For patients with limited lymph node involvement, chemotherapy can also be given post-surgery to kill any remaining cancer cells. This is known as adjuvant chemotherapy and helps prevent the chance of cancer recurrence.
For later stage cancers when surgery is no longer an option, chemotherapy is often administered with simultaneous radiation therapy. Known as combined chemoradiation therapy, this option often boasts survival rates higher than either treatment given alone or one after the other. This treatment is common if the cancer has spread to the mediastinal lymph nodes, which are located outside of the lung near the trachea and esophagus.
For early-stage small cell lung cancer patients in otherwise good health, doctors recommend combined chemoradiation therapy. Small cell cancers are highly responsive to chemotherapy, and survival is significantly improved when it is combined with early radiation therapy.
Once the cancer enters the extensive stage and spreads to distant organs, doctors typically prescribe a platinum-based chemotherapy regimen. This will involve platinum containing drugs like cisplatin or carboplatin with one or more additional chemotherapy drugs.
As many as 80%
The percentage of small cell lung cancer patients who may respond at least briefly to chemotherapy when the disease has already spread from the chest cavity (extensive stage disease).
Radiation is an effective treatment for non-small cell lung cancer. When applied in early stages for non-small cell lung cancer, radiation therapy is associated with 5-year survival rates between 13% and 39%. While radiation can help with local control, it’s much less effective for small cell lung cancer. This is especially true when it’s already spread extensively.
When lung cancer patients aren’t eligible for surgery, radiation is often recommended. High-energy targeted radiation stops cancerous cell division and reduces the size of tumors. The amount of radiation administered is thousands of times greater than the amount used in X-ray imaging, but treatment is divided into doses to limit the damage done to healthy tissues.
Like surgery, radiation therapy is a local treatment that only affects cells in the treatment area. Response rates for radiation therapy are significantly high, but relapse is common. As a result, it’s more often used palliatively. It’s administered in small doses to reduce pain where tumors have spread. It can also be given to prevent or treat lung cancers that spread to the brain.
Clinical trials test new drug combinations to improve treatment success rates while minimizing undesirable side effects. Many experimental or emerging lung cancer treatments are also used to treat other asbestos-related cancers such as mesothelioma, which develops on the lining of the lungs. Clinical trials for these treatments will often accept both lung cancer and mesothelioma patients.
A number of clinical trials studying combinations of immunotherapy and chemotherapy, targeted therapies and gene therapies are currently underway. Ask your doctor for more information about joining a clinical trial or speak with a Patient Advocate.
A 2021 study, for example, reported positive results combining photodynamic therapy with chemotherapy for lung cancer. Researchers reported improved disease control, reduced treatment resistance and increased overall effectiveness in cancer reduction compared to conventional options.

Access mesothelioma clinical trials matched to your diagnosis. Get help with eligibility and enrollment.
Get StartedIf you have been diagnosed with asbestos-related lung cancer, you’ll likely see more than one type of doctor. Leading cancer facilities recommend a multimodal approach to treatment, meaning several doctors specializing in different areas will work together to treat one patient.
Because lung cancer is so prevalent — the second-most diagnosed cancer in the United States — there is no shortage of doctors who treat it. The number of doctors who specialize in asbestos-related lung diseases is much smaller. Treating asbestos lung cancer comes with a special set of circumstances and challenges.
A growing number of well-regarded specialists who treat this disease are serving patients around the country. We can connect you with doctors such as thoracic surgeon Dr. Raphael Bueno, who is the associate chief of thoracic surgery at Brigham and Women’s Hospital in Boston, or Dr. James Luketich, who is chairman of the University of Pittsburgh Medical Center Lung and Esophageal Surgery Institute.

Boston, Massachusetts
Pleural Specialist | Thoracic Surgery
Expertise: Pleurectomy and Decortication Extrapleural Pneumonectomy
Languages: English

Pittsburgh, Pennsylvania
Pleural Specialist | Thoracic Surgery
Expertise: Minimally Invasive Surgery Research
Languages: English
With our network of more than 500 of the best mesothelioma specialists around the U.S., our Patient Advocates can help you find the right doctor for you. They also help with insurance, VA claims and answering questions you may have about clinical trials or available resources.
Recommended ReadingStay up-to-date on treatment, research, clinical trials, doctors and survivors
The information on this website is proprietary and protected. It is not a substitute for professional medical advice, diagnosis or treatment. Any unauthorized or illegal use, copying or dissemination will be prosecuted. Please read our privacy policy and terms of service for more information about our website.
This website and its content may be deemed attorney advertising. Prior results do not predict a similar outcome.
The Mesothelioma Center’s claim as the most trusted resource is based on our more than 150 5-star Google and BBB reviews. Our organization also helps more than half of all mesothelioma patients annually diagnosed.
Your web browser is no longer supported by Microsoft. Update your browser for more security, speed and compatibility.
If you are looking for mesothelioma support, please contact our Patient Advocates at (855) 404-4592
The Mesothelioma Center at Asbestos.com has provided patients and their loved ones the most updated and reliable information on mesothelioma and asbestos exposure since 2006.
Our team of Patient Advocates includes a medical doctor, a registered nurse, health services administrators, veterans, VA-accredited Claims Agents, an oncology patient navigator and hospice care expert. Their combined expertise means we help any mesothelioma patient or loved one through every step of their cancer journey.
More than 30 contributors, including mesothelioma doctors, survivors, health care professionals and other experts, have peer-reviewed our website and written unique research-driven articles to ensure you get the highest-quality medical and health information.
My family has only the highest compliment for the assistance and support that we received from The Mesothelioma Center. This is a staff of compassionate and knowledgeable individuals who respect what your family is experiencing and who go the extra mile to make an unfortunate diagnosis less stressful. Information and assistance were provided by The Mesothelioma Center at no cost to our family.LashawnMesothelioma patient’s daughter


Dixon, S. (2026, February 10). Asbestos-Related Lung Cancer Treatment. Asbestos.com. Retrieved March 3, 2026, from https://www.asbestos.com/cancer/lung-cancer/treatment/
Dixon, Suzanne. "Asbestos-Related Lung Cancer Treatment." Asbestos.com, 10 Feb 2026, https://www.asbestos.com/cancer/lung-cancer/treatment/.
Dixon, Suzanne. "Asbestos-Related Lung Cancer Treatment." Asbestos.com. Last modified February 10, 2026. https://www.asbestos.com/cancer/lung-cancer/treatment/.

Dr. Andrea Wolf is the Director of the New York Mesothelioma Program at Mount Sinai in New York City. She focuses on multidisciplinary treatment, clinical research, community outreach and education.
Our fact-checking process begins with a thorough review of all sources to ensure they are high quality. Then we cross-check the facts with original medical or scientific reports published by those sources, or we validate the facts with reputable news organizations, medical and scientific experts and other health experts. Each page includes all sources for full transparency.
Please read our editorial guidelines to learn more about our content creation and review process.
