“As a young woman with abdominal pain, I had a really hard time convincing someone I was in pain. A really hard time. I was told it was just my period,” Jayda said. Her doctors finally did a laparoscopy. Her peritoneal effusion turned out to be more than a gallon of fluid and the surgeon saw growths on her peritoneum. A biopsy confirmed her peritoneal mesothelioma diagnosis.
Peritoneal Effusion (Ascites)
Peritoneal effusion, or ascites, is a buildup of excess fluid in the abdomen. It can be caused by cirrhosis, liver diseases, peritoneal mesothelioma or other conditions. Doctors may treat peritoneal effusions with chemotherapy or by draining the fluid.
What Is Peritoneal Effusion?
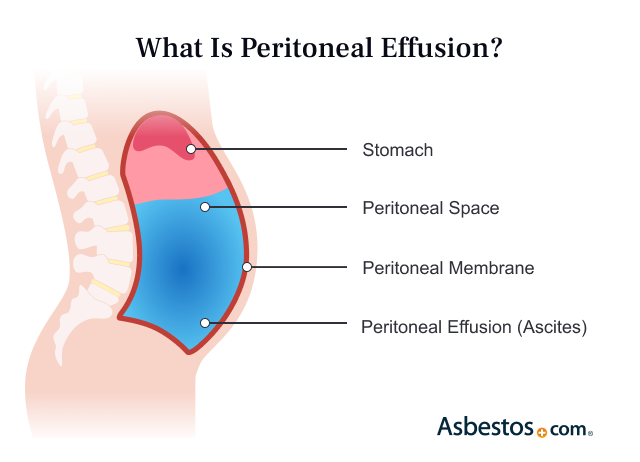
Peritoneal effusion is a buildup of fluid in the peritoneal cavity of people with peritoneal mesothelioma. This abnormal excess of fluid is also called ascites. When fluid accumulates in this space in the abdomen, it can cause the belly to swell. Excess fluid is common in those with peritoneal mesothelioma and liver issues.
The peritoneum is a thin membrane that lines the inside of the abdominal cavity. Conditions like cirrhosis or cancer can cause fluid to cross the peritoneum. When this happens, the fluid then collects in the peritoneal cavity. While ascites isn’t linked to mesothelioma survival rates, a worsening of pleural effusion is a sign of cancer progression.
Key Facts About Peritoneal Effusion
- Cirrhosis is the most common cause of ascites. It accounts for 80% of cases.
- Cancer is the second most common cause of ascites, with about 10% of cases.
- There are different types of pleural effusions. These include malignant and infectious.
- Recent research looked at fluid buildup and heated chemo in surgery. HIPEC treats recurring and cancerous effusions successfully.
There are different types of peritoneal effusions. They can be classified based on their cause. For example, cancer causes malignant peritoneal effusions. There are malignant and infectious ascites. They can also be classified based on their response to treatment. Uncomplicated effusions are easily treated. But refractory effusions are resistant to treatment.
Protein levels can also help classify ascites. An exudate is peritoneal fluid with a high protein level. A transudate is peritoneal fluid with a low protein level. This can help doctors find the cause of peritoneal effusion. Cirrhosis, or liver disease, usually causes low protein levels. Cancer and infections usually cause high levels.
What Causes Peritoneal Effusions?
Cirrhosis, or scarring of the liver, is the most common cause of ascites. Cirrhosis can cause high blood pressure in the liver’s veins. This can force fluid into the abdominal cavity.
Cancer, such as peritoneal mesothelioma, is the second most common cause of peritoneal effusions. Cancer cells can irritate the peritoneum. This can cause excess fluid to build up. Peritoneal mesothelioma tumors, for example, can cause the membrane to leak fluid. When any type of mesothelioma spreads, it can cause peritoneal effusions. Tumor spread, or metastases, to the lymph nodes can block the normal flow of lymph fluid.
Causes of Peritoneal Effusions and Percentage of Cases
- Cirrhosis or liver disease (about 81%)
- Cancer (about 10%)
- Heart failure (about 3%)
- Other causes (about 2%)
- Tuberculosis (about 2%)
- Dialysis (about 1%)
- Pancreatic disorder (about 1%)
Infections can also cause pleural effusions. Peritonitis can cause fluid to build up. Tuberculosis and pancreatitis, for example, are causes. Peritonitis can cause fluid to build up. It’s usually a bacterial infection. It can also be the result of fungus or a reaction to bile, stomach acid or dialysis solutions.
Heart or kidney failure can also cause ascites. When there’s less blood flow to the kidneys, fluid retention can happen. Heart failure can also affect the liver, making it more permeable. Fluid can then flow into the peritoneal cavity.

Understand your diagnosis, top doctors and ways to afford care.
Get Your Free GuideSymptoms of Peritoneal Effusion
The most common symptom of peritoneal effusion is discomfort. Swelling can cause pain. People also report feeling nausea and losing appetite. Symptoms can vary depending on the severity of the ascites and its cause.
Symptoms of Peritoneal Effusion
- Abdominal pain
- Abdominal swelling or distention
- Chest pain
- Fatigue
- Loss of appetite
- Nausea
- Swollen ankles
- Trouble breathing
- Weight gain
Peritoneal effusion is always a sign of a problem. It’s one of many signs and symptoms of mesothelioma. It occurs in more than 50% of peritoneal mesothelioma cases. It can also occur when other types of mesothelioma spread to the abdomen.
Dr. Anton Strocel, an OB/GYN who treated Trina Reif, spoke to us about her case. Trina is a 20-year peritoneal survivor. Dr. Strocel said, “Trina had unexplained ascites. We did an exploratory laparotomy. We also did multiple peritoneal biopsies. She had an angry looking peritoneum. Her diagnosis was abdominal mesothelioma.”
How Is Peritoneal Effusion Diagnosed?
Doctors use a mix of tests to diagnose peritoneal effusion. A physical exam and imaging scans are performed. Tests such as ultrasound and CT scans can show peritoneal fluid in the abdomen. A doctor will likely think of ascites if there is severe abdominal swelling.
If fluid is present, doctors need to collect a liquid biopsy. The key to a diagnosis is the laboratory analysis of the peritoneal fluid. The fluid is often collected during paracentesis. This procedure drains the fluid and collects it for analysis.
The sample is analyzed in a pathology lab. The type of peritoneal effusion is determined. Pathologists look for potential cancer cells. This process is known as cytology.
A 2022 study in journal Cytopathology looked at cytology testing of ascites fluid. It was able to detect malignant mesothelioma about 34% of the time. This underscores why doctors rely on biopsies. They can ensure an accurate mesothelioma diagnosis.
Treating Peritoneal Effusions
Draining the fluid treats noncancerous peritoneal effusions. Steps are also taken to prevent recurrence. For cancerous ascites, doctors may also use chemo. Pain management is usually offered for all types of ascites.
Mesothelioma treatments can ease peritoneal effusion symptoms. These treatments can also prevent recurrent effusions.
Paracentesis
Paracentesis for mesothelioma drains fluid. It’s a minor surgical procedure that uses a long, blunt needle. The doctor inserts the needle into the abdomen. Draining the fluid can relieve acute symptoms. It needs to be repeated if ascites returns.
Ascites can cause large volumes of fluid to build up in the abdomen. A recent study in The American Journal of Gastroenterology looked at effective ways to drain fluid. To keep protein and electrolyte levels in the blood normal, an infusion of albumin is needed
Intraperitoneal Catheter
For severe, recurring ascites, a surgeon can place a permanent catheter in the abdomen. A tube is attached to the catheter. This allows for constant drainage of the fluid.
This catheter is placed in a minor surgical procedure. Small incisions are made in the abdomen. An intraperitoneal catheter eliminates symptoms. It also ends the need for repeated paracentesis.
Chemotherapy
Chemo can improve malignant peritoneal effusions. It kills the cancer cells that produce ascites fluid. Ascites can recur when the cancer begins to regrow. Additional chemo can control recurring peritoneal effusions.
The Journal of Surgical Oncology published a study of malignant ascites in 2023. Researchers found combining treatments improved patient outcomes. Inpatient fluid draining, chemo and added nutrition had good results.
Cytoreductive Surgery and Heated Chemotherapy
Surgery and HIPEC effectively controls malignant ascites. Cytoreductive surgery removes cancerous tumors. Heated chemo in the abdomen kills remaining cells. This two-part procedure greatly reduces fluid production.
A 2023 study in the Journal of Obstetrics and Gynaecology tested a combo of treatments. HIPEC with targeted therapy was better than HIPEC alone. The study specifically tested bevacizumab.
Trials are testing pressurized intraperitoneal aerosolized chemo. PIPAC is expected to improve clinical outcomes,. This could especially help those who can’t have surgery.
Common Questions About Peritoneal Effusions
- Can peritoneal effusions be prevented?
-
You can take steps to prevent liver disease and some cancers. But that doesn’t guarantee you won’t get these diseases. A healthy lifestyle can lower your risk for cirrhosis. This includes avoiding alcohol and tobacco. Regular exercise and a healthy diet can improve health. Cutting back on salt can help reduce fluid retention.
- What are the complications associated with peritoneal effusions?
-
Peritoneal effusions can pressure the organs and chest. Persistent fluid in the abdomen can lead to infection. For example, spontaneous bacterial peritonitis can develop. Other complications include: Abdominal hernias, abdominal pain, difficulty breathing, fluid in the lungs and risk of infection.
- Are there any risk factors for developing peritoneal effusions?
-
Yes, riisk factors for peritoneal effusions include: Abdominal infections abdominal or pelvic cancer, alcohol abuse, congestive heart failure, genetic liver diseases, hepatitis B or C and nonalcoholic fatty liver disease. The biggest risk factors are conditions that lead to cirrhosis. Certain cancers and infections greatly increase risk. Heart or kidney failure also raise the risk of fluid in the abdomen.
- Can peritoneal effusions recur?
-
Yes, peritoneal effusions can, and often do, recur. Ascites can come back after treatment, depending on its cause. It can recur within days or months. In the case of malignant ascites, recurrent peritoneal effusions can be a sign of worsening cancer.
Recurrent ascites can be a sign of cancer like mesothelioma. If your peritoneal effusions persist, get a second opinion. A mesothelioma specialist may help.



