
Dr. Jacques Fontaine is a thoracic surgeon at Moffitt Cancer Center in Tampa, Florida, where he heads up the Mesothelioma Research and Treatment Center. He specializes in minimally invasive robotic surgery and aggressive surgeries for mesothelioma.
Testicular mesothelioma is the rarest asbestos-related cancer. It forms in the lining of the testes. Symptoms include a buildup of fluid and painful swelling of the testes. The 5-year survival rate for testicular mesothelioma is 49%.
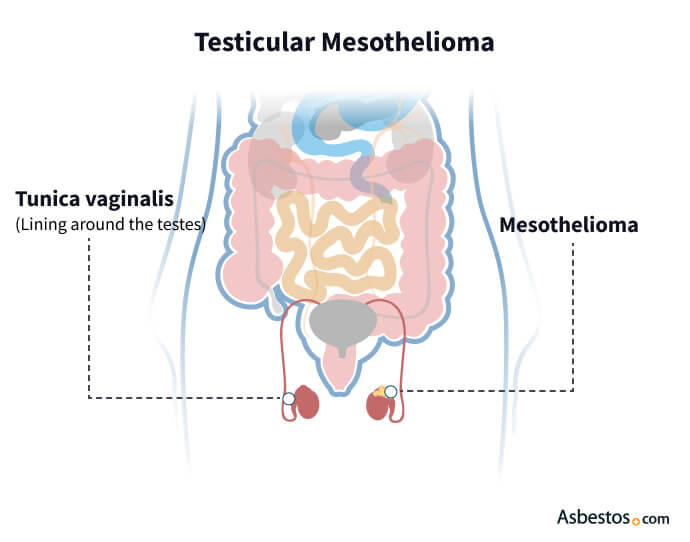
Testicular mesothelioma is a rare type of cancer that forms in the lining of the testes, known as the tunica vaginalis. Accounting for less than 1% of all mesothelioma cases, it’s linked to asbestos exposure, similar to pleural and peritoneal mesothelioma.
Key Facts About Testicular Mesothelioma
Learn about your diagnosis, top doctors and how to pay for treatment in our free mesothelioma guide.
Get Your GuideTesticular mesothelioma typically forms small tumors or nodules on the tunica vaginalis and often causes fluid buildup known as a hydrocele. Doctors have documented only a few hundred cases worldwide since the disease was first identified, underscoring its extreme rarity and the limited knowledge about its progression and clinical behavior compared to other mesothelioma types.
The most common symptoms of testicular mesothelioma are swelling or lumps in the testes, pain or discomfort in the scrotum and fluid buildup, known as hydrocele. These symptoms can be concerning and similar to those of other, less severe conditions, such as hernias or infections. This overlap can lead to misdiagnosis or delays in receiving the correct treatment.
Key Testicular Mesothelioma Symptoms
It’s important to seek medical attention if you experience any persistent symptoms, even mild ones. Early diagnosis is vital, leading to better treatment options and outcomes. If you or someone you know has a history of asbestos exposure and develops these symptoms, don’t hesitate to consult a healthcare professional.
Testicular mesothelioma primarily develops from asbestos exposure, similar to other forms of mesothelioma. However, its extreme rarity limits research into the exact connection between asbestos and this cancer.
Asbestos exposure happens when tiny fibers enter the body through inhalation or ingestion and cause severe health effects over time. Occupational risks include jobs in construction such as carpenters, military service including veterans who worked as mechanics or pilots, and industries like manufacturing, mining and shipbuilding.
Genetic predisposition or previous cancers may increase the risk of testicular mesothelioma among those exposed to asbestos but understanding of these links remains limited. Doctors still don’t fully understand how asbestos causes tumors to form specifically on the membrane that covers the testes. Unlike pleural or peritoneal mesothelioma, this type may have unique exposure or development patterns.
Doctors often diagnose testicular mesothelioma during or after surgery. Physical exams and imaging tests are often part of the diagnostic process, but a biopsy is the definitive way to confirm a mesothelioma diagnosis.
A biopsy involves removing a tissue sample from the tumor and sending it to the lab for testing. Staining of the sample helps doctors identify mesothelioma cells.
Standard Diagnostic Exams
Because it’s similar to other conditions like testicular cancer or benign cysts, many cases are often misdiagnosed. A biopsy is essential to rule out other testicular conditions. Early diagnosis improves patient outcomes.

We make getting expert care from the nation’s top mesothelioma specialists easy.
Find My SpecialistThe most common treatment for testicular mesothelioma is surgery. A 2023 research study noted testicular mesothelioma requires extensive resection, including metastatic surgery, if complete resection is possible. The study suggested a multimodality treatment plan offers the best outcomes.
Surgery may come before chemo with cisplatin and pemetrexed, the longstanding standard-of-care treatment for mesothelioma. Doctors may offer radiation therapy to kill any remaining cancer cells and prevent cancer from returning.
Testicular Mesothelioma Treatments
In some cases, testicular mesothelioma is a secondary tumor, with the primary tumor located within the peritoneum (the membrane that lines the abdominal cavity). In these situations, doctors must treat the patient for peritoneal mesothelioma cancer.
Treating testicular mesothelioma requires a specialized approach. Treatment plans are tailored to each person and factors like the stage of cancer, the person’s overall health and the potential for surgery.
Testicular mesothelioma is extremely rare, making it difficult to collect comprehensive data on outcome (prognosis) and survival. Prognosis refers to the likely course of a disease, while survival rates show the percentage of people who live for a specified time after diagnosis.
In one large review of testicular mesothelioma published in Urology, about 49% of people lived at least 5 years and about 33% lived 10 years. However, older studies show median survival around 2 years in many cases. Many factors, including stage, age, overall health and treatment, affect the outcome.
Testicular mesothelioma can spread quickly. Although tumors are often surgically removed, the cancer tends to recur within a few years. Still, men with testicular mesothelioma generally have a significantly better prognosis than most people with other mesothelioma types.
Testicular mesothelioma patients I’ve spoken with are usually concerned about the rarity of this diagnosis. Some patients seem to have a longer life expectancy and better quality of life compared to patients with other types of mesothelioma.
The stage when testicular mesothelioma is diagnosed plays a critical role in prognosis. Early detection, when the cancer is still limited to the tunica vaginalis, usually leads to a better outlook. In contrast, late-stage diagnosis, when the cancer has spread to nearby organs or lymph nodes, tends to have a less favorable prognosis. Because testicular mesothelioma is rare, many cases are diagnosed early, which can improve outcomes.
Younger people and those with good overall health generally respond better to treatment. A strong immune system helps manage aggressive therapies such as chemo and surgery. For example, patients under 50 often show better responses. Survivor stories often highlight the value of maintaining good health during treatment.
Regular follow-up visits are essential to track how well treatments work and to catch early signs of recurrence. Monitoring offers important information on a patient’s progress and helps guide any needed changes in treatment.
How well a person responds to treatments, including surgery, chemo and immunotherapy, greatly impacts prognosis. Positive treatment results can boost survival rates and improve quality of life.
Testicular mesothelioma specifically affects the lining of the testes, while testicular cancer originates in the testicular tissue itself. Both can present similar symptoms, but they’re distinct diseases requiring different treatment approaches.
If you’ve been exposed to asbestos and experience symptoms such as swelling or discomfort in the testes, it’s essential to seek medical attention immediately. Early diagnosis is critical for better treatment outcomes.
Yes, like other cancers, testicular mesothelioma can metastasize or spread to nearby organs and lymph nodes. This is why early detection and treatment are crucial.
Yes, individuals diagnosed with testicular mesothelioma from asbestos exposure may be eligible for financial compensation. It’s advisable to consult with a legal expert specializing in asbestos-related cases to explore your options.
Stay up-to-date on treatment, research, clinical trials, doctors and survivors
The information on this website is proprietary and protected. It is not a substitute for professional medical advice, diagnosis or treatment. Any unauthorized or illegal use, copying or dissemination will be prosecuted. Please read our privacy policy and terms of service for more information about our website.
This website and its content may be deemed attorney advertising. Prior results do not predict a similar outcome.
The Mesothelioma Center’s claim as the most trusted resource is based on our more than 150 5-star Google and BBB reviews. Our organization also helps more than half of all mesothelioma patients annually diagnosed.
Your web browser is no longer supported by Microsoft. Update your browser for more security, speed and compatibility.
If you are looking for mesothelioma support, please contact our Patient Advocates at (855) 404-4592
The Mesothelioma Center at Asbestos.com has provided patients and their loved ones the most updated and reliable information on mesothelioma and asbestos exposure since 2006.
Our team of Patient Advocates includes a medical doctor, a registered nurse, health services administrators, veterans, VA-accredited Claims Agents, an oncology patient navigator and hospice care expert. Their combined expertise means we help any mesothelioma patient or loved one through every step of their cancer journey.
More than 30 contributors, including mesothelioma doctors, survivors, health care professionals and other experts, have peer-reviewed our website and written unique research-driven articles to ensure you get the highest-quality medical and health information.
My family has only the highest compliment for the assistance and support that we received from The Mesothelioma Center. This is a staff of compassionate and knowledgeable individuals who respect what your family is experiencing and who go the extra mile to make an unfortunate diagnosis less stressful. Information and assistance were provided by The Mesothelioma Center at no cost to our family.LashawnMesothelioma patient’s daughter


Asbestos.com. (2026, January 28). Testicular Mesothelioma. Retrieved February 7, 2026, from https://www.asbestos.com/mesothelioma/testicular/
"Testicular Mesothelioma." Asbestos.com, 28 Jan 2026, https://www.asbestos.com/mesothelioma/testicular/.
Asbestos.com. "Testicular Mesothelioma." Last modified January 28, 2026. https://www.asbestos.com/mesothelioma/testicular/.

Dr. Jacques Fontaine is a thoracic surgeon at Moffitt Cancer Center in Tampa, Florida, where he heads up the Mesothelioma Research and Treatment Center. He specializes in minimally invasive robotic surgery and aggressive surgeries for mesothelioma.
Our fact-checking process begins with a thorough review of all sources to ensure they are high quality. Then we cross-check the facts with original medical or scientific reports published by those sources, or we validate the facts with reputable news organizations, medical and scientific experts and other health experts. Each page includes all sources for full transparency.
Please read our editorial guidelines to learn more about our content creation and review process.
