Clinical Trials Lead to Promising Updates in Mesothelioma Immunotherapy
Research & Clinical TrialsWritten by Sean Marchese, MS, RN | Edited By Walter Pacheco
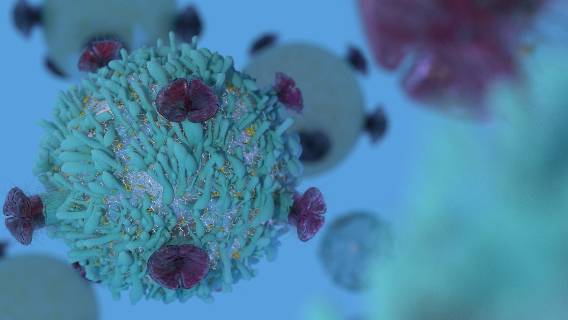
Researchers have made significant progress in mesothelioma treatment advancements recently, including promising work with immunotherapy.
The first U.S. Food and Drug Administration-approved combination immunotherapy for mesothelioma, nivolumab and ipilimumab, known by brand names Opdivo and Yervoy, has been effective for many patients.
In September 2021, the European Society for Medical Oncology presented study data showing a three-year survival rate of 23% for mesothelioma patients on Opdivo and Yervoy. By comparison, the three-year survival rate for chemotherapy patients was 15%.
However, some patients cannot receive immunotherapy drugs due to chronic medical conditions or a lack of specific biomarkers. Immunotherapy is also not a final solution to mesothelioma. For example, Opdivo and Yervoy are only available as a first-line treatment for mesothelioma patients, not if cancer returns after prior treatment.
In many cases, current immunotherapy can improve survival compared to traditional methods, but there’s still room for improvement. The most effective treatments for mesothelioma include a multimodal approach combining immunotherapy with surgery, chemotherapy, radiation or other procedures.
5 Promising Mesothelioma Immunotherapy Advancements
In November, Dr. Anna Nowak, a researcher at the Institute for Respiratory Health in Perth, Western Australia, published her team’s report on updates to the latest immunotherapy trials for mesothelioma.
Nowak’s focus is immune checkpoint inhibitor therapy, the same class of drugs as Opdivo and Yervoy. Also known as checkpoint blockades, these treatments hold significant potential for improving pleural mesothelioma prognosis and life expectancy.
“The most impressive advancement for checkpoint blockade has been the demonstration that for people with sarcomatoid and biphasic mesothelioma, we can double survival with the combination of ipilimumab and nivolumab,” Nowak told The Mesothelioma Center at Asbestos.com.
This recent study provided an overview of recent clinical trials for malignant pleural mesothelioma and highlighted the most promising new advancements in immunotherapy.
- Second-Line Nivolumab: The randomized CONFIRM study recruited 332 participants who had failed one or two previous lines of therapy. Both pleural and peritoneal mesothelioma were eligible. Second-line nivolumab alone improved overall survival from 6.9 months to 10.2 months compared to the placebo group. Median progression-free survival was three months.
- Anti-CTL4 and Anti-PD-L1 Combinations: The phase II NIBITMeso trial tested the anti-CTLA4 agent tremelimumab with the anti-PD-L1 agent durvalumab (Imfinzi) as a first-line or second-line therapy. Of the 40 participants, 65% of patients had disease control. The INITIATE study tested first-line nivolumab and ipilimumab in 38 patients, with 68% showing disease control.
- Chemoimmunotherapy with Checkpoint Blockade: Results of the PrE0505 study support the potential of combining chemotherapy with checkpoint blockade or inhibitors. This 55-patient study combined the chemotherapy drugs cisplatin and pemetrexed with durvalumab. The median overall survival was 20.4 months, and the median progression-free survival was 6.7 months.
- Biomarker Testing for Checkpoint Blockade: Recent evidence suggests that testing for PD-L1 biomarker expression is not a good indicator of success for anti-PD-L1 immunotherapies such as pembrolizumab (Keytruda). However, new studies show that monitoring PD-L1 with radioactive tracers provides a more practical, real-time level of biomarker activity.
- Proper Sequencing of Immunotherapies: There is limited data on immunotherapy patients who receive treatment before or after other therapies. However, the CheckMate 743 trial indicated that neoadjuvant use could effectively reduce tumor bulk before surgery for mesothelioma. Several pilot clinical trials are examining both adjuvant and neoadjuvant checkpoint blockade.
Some mesothelioma cell types, such as epithelioid, respond less well to immunotherapy. Nowak believes more research will reveal new options for these patients.
“This is why we need to support the clinical trials that will answer this question,” she said. “I am optimistic that the combination of chemotherapy and checkpoint blockade may do for epithelioid mesothelioma what dual checkpoint blockade has done for non-epithelioid mesothelioma.”
Anti-Angiogenesis Becoming a New Standard for Immunotherapy
Scientists continue to study new drugs and mesothelioma treatments that improve overall survival and safety for more people. A 2021 study in the Journal of Cancer Metastasis and Treatment recently evaluated several ways mesothelioma immunotherapy is evolving.
In addition to Opdivo and Yervoy for unresectable malignant pleural mesothelioma, scientists are researching other immunotherapy combinations. One method that has shown effectiveness is anti-angiogenesis, a type of immunotherapy that targets blood vessels.
Angiogenesis is the process of new blood vessel formation. In cancer, tumors form blood vessels to use oxygen for growth and metastasis. Anti-angiogenesis medications inhibit vascular endothelial growth factors, or VEGF. These drugs prevent new blood vessel growth, effectively starving tumors of oxygen and nutrients.
A popular VEGF inhibitor for mesothelioma, bevacizumab, was recently part of a large, phase III randomized controlled trial conducted by the French thoracic oncology cooperative group IFCT. This study recruited patients with unresectable pleural mesothelioma who had not received prior chemotherapy.
The primary endpoint of median overall survival was significantly longer with the addition of bevacizumab to chemotherapy at 18.8 months versus 16.1 months with chemotherapy alone. However, adverse events such as hypertension and bleeding were more common in the bevacizumab group.
More recently, studies such as the phase II RAMSES trial in 2020 have shown promising results for combining anti-VEGF medication with chemotherapy as a second-line treatment. The addition of the VEGF inhibitor ramucirumab significantly improved median overall survival to 13.8 months compared to 7.5 months for chemotherapy alone.
Future clinical trials will undoubtedly build on the success of current immunotherapies, including VEGF-inhibitors, checkpoint blockades and more. In 2022, researchers will hopefully find ways to improve the effectiveness, response rate and safety of these therapies for mesothelioma patients.