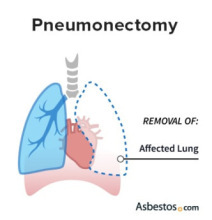
Pneumonectomy
A pneumonectomy is the surgical removal of a lung. It is a major procedure that aims to entirely remove a lung when cancer, such as mesothelioma, is diagnosed in or on that lung. Performing a pneumonectomy can prevent the spread of malignant cells to other sites in the body.
What Is a Pneumonectomy?
Pneumonectomy is an intensive surgery that removes one or more lung lobes or an entire lung. Surgeons may perform a pneumonectomy for mesothelioma because it is not possible to remove asbestos from the lungs.
This procedure also treats other lung cancers, chest conditions and injuries. You may receive a pneumonectomy in addition to other cancer treatments, such as radiation therapy and chemotherapy.
A standard pneumonectomy is a type of surgery that removes an entire lung. While there is an expanded type of this surgery, a simple pneumonectomy removes only the lung itself.
Extrapleural pneumonectomy removes the entire lung in addition to the lining of the lung (pleura), heart lining (pericardium), diaphragm and nearby lymph nodes. Surgeons usually reserve an EPP for patients with advanced mesothelioma or lung cancer.
- Pneumonectomy is a high-risk procedure.
- Malignant lung diseases are the most common indication for pneumonectomy.
- A comprehensive study at a German hospital between 2014 and 2022 found the 90-day mortality was 17.2%.
Should You Consider a Pneumonectomy?
When deciding whether to consider a pneumonectomy, surgeons look at the type of cancer, its location and how far it has spread. This procedure is usually performed in patients with tumors along the main airway (bronchus) or along divisions between lung lobes (fissures). Surgeons also need to consider whether the patient is healthy enough for surgery by performing lung function tests.
- Extensive thymomas (thymus tumors)
- Inflammatory lung disease
- Lung trauma
- Mesothelioma
- Non-small cell lung cancer
It is necessary to weigh the risks and benefits when deciding whether to perform a pneumonectomy or a less intensive surgery. One study found that within 30 days of surgery, patients were three times as likely to die after pneumonectomy (9.6%) than sleeve lobectomy (3.2%).

Although a pneumonectomy may seem extreme, an experienced mesothelioma surgeon would decide whether the benefits outweigh the risks for this aggressive procedure. Pre-op testing would help the surgeon make that decision.
What Can I Expect From a Pneumonectomy Procedure?
Before the pneumonectomy procedure, you should expect tests that check lung function because a pneumonectomy is an intensive surgery. You should also expect the doctor to perform a thoracic epidural beforehand to control pain after the surgery.
Patients undergo a pneumonectomy under general anesthesia. The surgeon begins with a thoracotomy, in which they make a long incision on the same side of the chest as the diseased lung. They may remove part or all of a rib to get a better view of the lung.
Patients undergo a pneumonectomy under general anesthesia. The surgeon begins with a thoracotomy, in which they make a long incision on the same side of the chest as the diseased lung. They may remove part or all of a rib to get a better view of the lung.
The surgeon then collapses the affected lung and staples, clamps or ties off any attached blood vessels. They do the same to the bronchus or the main airway in the lung and then can remove the diseased lung through the incision. The surgeon checks the cut vessels and tubes for any signs of leakage. They also place a temporary drainage tube to draw air, fluid and blood out of the surgical cavity before closing the chest incision.
Surgeons can choose to perform video-assisted thoracoscopic surgery (VATS) or robotic-assisted thoracoscopic surgery (RATS). These procedures are minimally invasive and require a much smaller incision to access the diseased lung. VATS and RATS have a shorter recovery time compared to thoracotomy, but it is not always possible to perform them.
Pneumonectomy Recovery
After a pneumonectomy, patients initially recover in the hospital’s intensive care unit. In rare cases, they may need a respirator for one or two days after the operation to assist with breathing. Some patients may also need oxygen therapy to maintain their blood oxygen levels. The drainage tubes will remain in place to monitor for bleeding and air leakage.
- Encouraging a patient to cough up accumulated lung secretions
- Helping the patient walk to prevent the formation of blood clots
- Monitoring blood oxygen levels
- Relieving pain
A full recovery from a pneumonectomy may take as long as two or three months. During this time, patients can slowly start to add more non-strenuous activities to their daily routine and return to work if possible. Some patients who have had a pneumonectomy experience shortness of breath for up to six months after their procedure.

Connect with trusted specialists who truly care about your health. Get fast, stress-free appointment help.
Find a Doctor NowPneumonectomy Risk Factors and Complications
Common pneumonectomy complications include pneumonia, possible kidney failure and heart problems among others. Your doctor will help you weigh the risks and benefits of a pneumonectomy and how it can affect your prognosis. It is important to follow all post-surgery instructions to heal properly and avoid complications.
- Acute respiratory distress syndrome
- Bronchopleural fistula (an abnormal fusion of the stump of the cut bronchus and the pleural space)
- Heart problems, such as cardiac arrhythmia (abnormal heart rhythm) and myocardial infarction (heart attack)
- Kidney or other organ failure
- Pneumonia
- Pulmonary edema (fluid accumulation in the lungs)
- Pulmonary embolism (blood clot) in the remaining lung
- Postpneumonectomy cardiac herniation (movement of the heart through a hole in the outer muscle wall)
- Postpneumonectomy empyema (infection of the pleural cavity and accumulation of pus in the pleural space)
- Postpneumonectomy syndrome (other organs in the chest moving into the empty space of the removed lung)
- Prolonged need for a respirator
The prognosis following a pneumonectomy depends on many factors. They include the lung to be removed, the type and stage of the patient’s cancer, and the patient’s gender, age and overall health.
Pneumonectomy Outcomes and Success Rates
Pneumonectomy has a high mortality rate and is often associated with a worse prognosis than other surgeries. One study reported the median survival following a pneumonectomy was 23.6 months, compared to 60.7 months for those who received a sleeve lobectomy. This means half of the patients who underwent a pneumonectomy lived less than two years after their surgery.
Complication rates are also higher in pneumonectomy patients. Another study of 145 patients who had the procedure found that 41.4% experienced complications. Common events included arrhythmias and second operations to control bleeding.
Some research shows that minimally invasive surgeries are safer and as effective as a standard pneumonectomy. Surgeons can collect the tissue samples and remove cancerous tissues with the same success rates. Patients also have shorter hospital stays after VATS compared to a standard pneumonectomy.
Common Questions About Pneumonectomy
- What is the difference between a standard pneumonectomy and an extrapleural pneumonectomy?
-
During a standard pneumonectomy, the surgeon only removes the diseased lung. In an extrapleural pneumonectomy, the entire lung is removed in addition to some surrounding tissues and structures. The goal of an EPP is to remove as much cancerous tissue from the chest cavity as possible.
- Is a sleeve lobectomy the same as pneumonectomy?
-
No, a sleeve lobectomy is not the same as a pneumonectomy. During a sleeve lobectomy, the surgeon removes only part of the diseased lung while preserving the rest of the unaffected tissue. This procedure is less intensive than a pneumonectomy because it removes less lung tissue.
- Can pneumonectomy be part of a multimodal treatment plan for mesothelioma?
-
Yes, surgeons use pneumonectomy as part of a comprehensive treatment plan for mesothelioma and other lung cancers. Studies show that pneumonectomy is effective when used alongside chemotherapy, targeted therapy and immunotherapy. Doctors may give these treatments before surgery to shrink tumors or after surgery to kill any cancer cells left behind.




