Robotic Surgery for Mesothelioma
A robotic surgery system can enhance the abilities of a surgical team, allowing them to perform an aggressive mesothelioma surgery more safely. Currently, only a handful of advanced cancer centers in the United States offer this option to mesothelioma patients.
What Is Robotic Surgery?
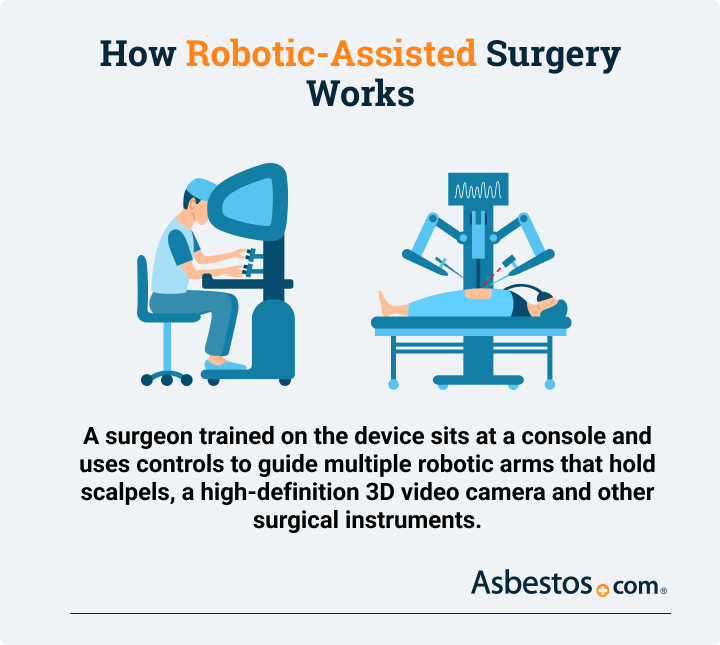
Robotic surgery, or robot-assisted surgery, is any surgical procedure involving a robotic system with a camera, mechanical arms and surgical instruments attached to them. This type of surgery often only requires tiny incisions but can also be helpful during open or more invasive surgeries.
The robotic systems mesothelioma specialists use don’t involve artificial intelligence. They’re superior tools to help expert human surgeons. The surgeon’s view is also projected onto screens in the operating room so the entire surgical team can collaborate during surgery.
Several accomplished mesothelioma doctors have begun to advocate for robotic technology. Robotic surgery is becoming a vital tool in mesothelioma treatment, with top specialists leading the charge of enhancing precision and reducing patient recovery times. These experts are pioneering minimally invasive procedures that offer promising outcomes and advancing the accessibility of robotic-assisted surgery for mesothelioma care.
Surgeons have used robotic tools for chest cancer procedures since 2006. The first robotically assisted EPP was conducted in 2013 using the da Vinci Surgical System.
How Does Robotic Surgery for Mesothelioma Work?
When using robotic surgery for mesothelioma, the surgeon controls the mechanical arms remotely. The control center or central console is near the operating table. The cameras allow the surgeon to see a magnified and clear view of the surgical site. The surgeon also leads nurses and surgical assistants during the operation.
- You’ll be put under anesthesia and the surgical team prepares the room and instruments.
- Your surgeon creates one or more tiny incisions in your body.
- Your doctor inserts a small portion of the robotic instrument with a camera into the insicion.
- Your doctor sits at the control console and directs the operation using remote controls and a high-quality camera feed.
- The robotic arms and tools translate the input into small and precise movements, which are more accurate and fluid than a human hand.
Innovative robots such as the da Vinci Surgery System are designed to minimize the harmful side effects of surgery. Robotic surgery is an evolved form of video-assisted thoracoscopic surgery. A surgeon uses long, thin tools and a camera on a probe to see what they’re doing without completely opening the chest. Many specialists rely on VATS to perform biopsy procedures as part of a mesothelioma diagnosis.
VATS isn’t ideal for more complex procedures. The 2D camera eliminates the surgeon’s depth perception, and the tools are counterintuitive. A robotic surgery system solves these problems, giving the surgeon a magnified 3D view. It translates the surgeon’s movements into precise movements of tiny robotic hands. The surgeon can adjust the sensitivity of the controls as needed. The system filters out any tremors in the surgeon’s fingers.

Get a free guide with the latest mesothelioma treatments and clinical trials.
Get Yours NowWhat Are the Benefits of Robotic Surgery for Mesothelioma?
One of the benefits of using robotic surgery is an improvement of aggressive tumor-removing surgery. An extrapleural pneumonectomy is a good example. EPP procedures carry significant risks during surgery for pleural mesothelioma. During an EPP, surgeons remove the diseased lung, parts of the lining surrounding the heart and chest, nearby lymph nodes and part of the diaphragm if necessary. EPP involves a difficult recovery period. Surgeons often discover patients are poor candidates for surgery only after making a considerable incision to open the chest.
When we interviewed Dr. Marcelo DaSilva, chief of thoracic surgery and medical director at AdventHealth Cancer Institute, he said his treatment center combines “intraoperative heated chemotherapy technique with minimally invasive measures, such as robotic surgery for mesothelioma, to reduce side effects and potential complications for patients.”
Mesothelioma Robotic Surgery Advantages
- Better Patient Selection: Enables better preoperative evaluation of cancer spread, allowing surgeons to thoroughly look around inside the patient’s body before making a final decision to go ahead with performing more invasive procedures.
- Improved Cancer Cell Removal: The very fine instrumentation and 3D-magnified view inside the patient’s body allows for very precise movements to locate and remove cancer growth much more accurately.
- Reduced Blood Loss: With robotic tools, the doctor can stop any bleeding during aggressive tumor-removing surgery much faster. This means that patients need to stay in the hospital for a few days instead of weeks.
According to ScienceDirect, in robotic surgery, a surgeon uses remote-controlled surgical tools and sees inside the patient’s body through a 3D camera. The tools and camera are mounted on little robotic arms that can fit through small incisions in the patient’s chest.
Robotic surgery helps doctors look at how much the tumor has grown and stops a lot of bleeding. This means that people who can’t be helped with surgery don’t have to go through a long operation, while those who can benefit have an easier recovery.
It’s not a robot performing the surgery. A surgeon performs the procedure with very fine movements and very fine instruments. We make little cuts between the ribs or on the belly, and insert a 3D camera and instruments. Then we use a console with 3D vision and very fine controllers to move the instruments around.
Robotic Surgery Risks
A risk of robotic surgery is the high cost of the technology, which may hinder hospitals and cancer centers that cannot afford the pricey equipment. However, if patients spend fewer days recovering in a hospital bed, a surgical practice can realize great savings in the long run.
Additionally, the technology isn’t yet widespread. Patients still have to travel to one of a handful of advanced cancer centers around the country to find a surgeon with experience treating mesothelioma through robotic surgery.
Recommended Reading



