Mesothelioma in Young Adults & Children
Mesothelioma is very rare in children and young adults. The cancer usually develops decades after exposure to asbestos. Mesothelioma cases in young people account for 2% to 5% of all diagnoses.
What Causes Mesothelioma in Children and Young Adults?
There is no clear cause for mesothelioma in young people. The disease is spontaneous, though possible factors include toxic exposure or genetic disorders.
Mesothelioma is a rare cancer that tends to appear in people over 65. Only a few hundred cases have been reported in young adults and children worldwide.
Possible Causes of Mesothelioma in Young Adults and Children
- Exposure to asbestos in products, the environment or through a family member.
- Radiation exposure, including radiation therapy for other cancers.
- In utero exposure to the antibiotic isoniazid, which is a tuberculosis treatment.
- Genetic predisposition to mesothelioma.
The primary cause of this cancer in adults is occupational asbestos exposure. Most young people diagnosed with mesothelioma have no history of asbestos exposure. Asbestos-related illnesses take several decades to develop after exposure.
“From what I have seen, there is limited data on childhood mesothelioma,” says Karen Selby, a registered nurse and Patient Advocate at The Mesothelioma Center. “There have been fewer than 300 cases ever reported, which limits our ability to have many facts.”
How Are Children Exposed to Asbestos?
Asbestos exposure generally endangers adults working in certain jobs or the military. Children encounter asbestos exposure in other ways.
Researchers have looked for other potential causes in children and young adults. Mesothelioma in youth is so rare that it’s challenging to study.
“In my experience here at The Mesothelioma Center, I’ve only assisted one patient under the age of 18,” Karen Selby says. “In this particular case, there was no known exposure to asbestos, and the cause was considered unknown.”
Children’s Products Containing Asbestos
Asbestos-contaminated talc has found its way into many products for children. Examples include crayons, clay, toys and children’s cosmetics. Talcum powder and baby powder brands have contained asbestos as well.
Claire’s and Justice, brands that sell products for teenagers, recalled several children’s makeup kits over asbestos contamination in 2017. The U.S. Food and Drug Administration confirmed the test results in 2019.
The Environmental Working Group Action Fund performed independent tests in 2015. They found asbestos in crayons and toy crime lab kits made in China.
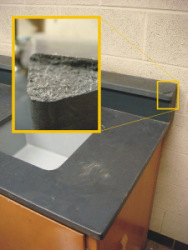
Asbestos in Homes and Schools
In the U.S., old asbestos construction materials are in many older buildings. Millions of homes and 50% of America’s schools contain asbestos products from the 1950s and 1960s. Any activity that disturbs deteriorating asbestos products can release toxic asbestos dust into the air.
Austin Lacy, for example, was a high school football star in Pasadena, California. For nearly a year, doctors couldn’t find the cause of his health decline before he was diagnosed with mesothelioma. Sadly, he died just 10 days before graduation. Asbestos in public schools may have contributed to his disease.
Boston resident Kevin Morrison was diagnosed with peritoneal mesothelioma at 21. The former high school athlete likely encountered old asbestos products in school and public buildings. The Boston area has many old buildings containing asbestos.
Builders once commonly used asbestos materials before they were phased out in the late 1980s. Boiler insulation, ceiling tiles, duct wrap for HVAC systems, pipe insulation, vinyl flooring (including backing and glue) and wallboard all often contained asbestos.
Secondhand Exposure
Asbestos exposure at work can lead to secondhand exposure at home. If workers bring asbestos dust home, it can harm their families. Sources of secondary exposure include contaminated work clothes, hair or tools.
At 31, Jayda Kelsall was diagnosed with peritoneal mesothelioma. She was most likely exposed to asbestos as a child through her father. He used and tested asbestos products in a coal mine lab. Fortunately, Kelsall was eligible for surgery and chemotherapy. “If I had given up when they first told me, ‘Oh, it’s just a little period pain,’ I might not be here today,” Kelsall says.
Before the 1970s, the risk of secondary asbestos exposure was higher. Today, laws require employers to offer decontamination facilities for asbestos workers.
Environmental Exposure
Children may be exposed to asbestos in areas where it’s found in the water, air or soil. Residents in communities where asbestos was mined or asbestos products were produced were also at risk.
In Libby, Montana, children played on soil from asbestos mine tailings. In Ambler, Pennsylvania, they played on piles of asbestos factory waste.

Understand your diagnosis, top doctors and ways to afford care.
Get Your Free GuideSymptoms of Mesothelioma in Children and Teens
The most common mesothelioma symptoms are fatigue, weight loss and pain. Regardless of a patient’s age, the symptoms of mesothelioma are usually the same.
The initial signs can often be confused with more common illnesses. Identifying symptoms is also challenging when children have difficulty describing how they feel. Pediatric doctors and nurses use age-appropriate communication to connect with children. They teach them how to recognize and describe changes in their bodies.
Mesothelioma Symptoms in Young People
- Peritoneal Mesothelioma: Digestive problems, abdominal pain, fatigue and weight loss.
- Pleural Mesothelioma: Breathing problems, chest pain, fatigue and weight loss.
Some research shows mesothelioma spreads faster in children than in adults. This means symptoms may progress more quickly in children compared to adults.
Diagnosing mesothelioma in children is challenging because of its nonspecific symptoms and rarity. Doctors prioritize ruling out more common pediatric conditions. It’s also important to differentiate mesothelioma from other pediatric cancers, such as sarcomas or Wilms tumor.
How Are Children Diagnosed With Mesothelioma?
Doctors use a combination of tools to confirm a mesothelioma diagnosis in children and teens. While the diagnostic tools used are the same, the process is more cautious and collaborative to accommodate the unique needs of pediatric patients.
Accurate diagnosis often requires collaboration among specialists. Pediatric oncologists, radiologists and pathologists work together to differentiate mesothelioma from other conditions.
Diagnostic Tools
- Physical Exam: Doctors perform lung function tests and feel for tumors under the skin.
- Imaging Scans: These tests detect fluid buildup or abnormalities in the chest or abdomen. They’re adjusted to minimize radiation exposure in children while still capturing detailed images.
- Fluid Analysis: Cytology tests examine pleural or peritoneal fluid for cancer cells.
- Biopsy: Pathologists examine tissue samples under a microscope to confirm mesothelioma. Biopsy techniques are often less invasive and carefully planned to reduce risks given children’s smaller bodies and sensitivity to procedures.
A 2021 case study of a 14-year-old boy with peritoneal mesothelioma showed radiology can help diagnose rare cases in children. An interventional radiologist helped diagnose the case with an ultrasound-guided core biopsy and diagnostic paracentesis.
According to the CDC, 0.3% of patients diagnosed in 2021 were between 45-54 years old. No one under 45 received a diagnosis that year, which is the most recent year for which this data is available. A review of thousands of patients in 2015 found only 2% were under 40.
Asbestos Exposure History Can Aid Diagnosis
It’s important to tell your doctor about any potential history of asbestos exposure. This information can help prompt your doctor to test for certain cancers.
Young people with mesothelioma don’t always have a history of asbestos exposure. Children may have a genetic predisposition to mesothelioma if they’re born with certain mutations in their DNA.
A couple of recorded cases of pediatric mesothelioma are linked to receiving radiation therapy for a disease called Wilms’ tumor. Childhood mesothelioma has been linked to exposure to isoniazid, an antibiotic used to treat tuberculosis, while in the womb.
Mesothelioma Treatment for Children and Young Adults
Young patients get the same types of mesothelioma treatment as adults. However, cancer treatment in children requires adjustments for their smaller size and developing bodies.
Types of Treatment
- Chemotherapy: The most common is chemotherapy with Alimta (pemetrexed) and cisplatin. Doctors adjust the dose based on a child’s weight and size.
- Clinical Trials: Your pediatric oncologist may know of a clinical trial appropriate for children or teens.
- Immunotherapy: Little data is available about immunotherapy for childhood mesothelioma. Doctors believe it’s generally safe to treat pediatric cancer.
- Radiation Therapy: Radiation therapy uses lower, more precise doses to avoid harming growth.
- Surgery: Younger patients are more likely to qualify for tumor-removing surgery. This surgery significantly boosts their chance of long-term survival.
Pediatric specialists focus on minimizing long-term effects while effectively managing the disease. For example, doctors will plan treatment to lower the risk of secondary cancers later in life.

Connect with trusted specialists who truly care about your health. Get fast, stress-free appointment help.
Find a Doctor NowYounger vs. Older Mesothelioma Patients
Younger mesothelioma patients often have better overall health, fewer coexisting conditions and stronger responses to aggressive treatments. These factors may result in improved survival.
| Patients under age 40 | Patients older than age 40 | |
|---|---|---|
| Relative Incidence | 2% of study population | 98% of study population |
| Patient Gender | 51% male, 49% female | 78% male, 22% female |
| Type of Mesothelioma | 47% pleural, 48% peritoneal | 90% pleural, 9% peritoneal |
| Median Survival | 34 months | 8 months |
| Five-Year Survival Rate | 38% | 3% |
Researchers from the National Institutes of Health studied 12,345 mesothelioma patients. They discovered some differences among the small fraction of patients under 40. There was little difference in the incidence for each gender and the 2 main types of mesothelioma.
Younger patients have a longer median survival and a higher 5-year survival rate. This is primarily because older patients usually have additional health problems that interfere with their cancer treatment.
Tips for Protecting Your Child from Asbestos Exposure
Taking proactive steps can help safeguard your child’s health and reduce the likelihood of asbestos exposure. Any home or school built before 1980 is likely to contain asbestos.
Tips to Prevent Asbestos Exposure in Children
- Avoid disturbing materials that may contain asbestos, such as old insulation, ceiling tiles or pipe wraps.
- Inspect your home for signs of damage to asbestos-containing materials. Hire licensed professionals for asbestos testing and removal in your home if necessary.
- Prevent access to home renovation areas where asbestos may be present.
- Ask administrators at your child’s school about asbestos safety regulations to ensure compliance with the law.
- Avoid products with talc such as makeup kits, clay, crayons and fingerprint kits.
It’s important to stay informed about local environmental risks, such as contaminated soil or natural asbestos deposits. Remove children from areas with asbestos, change their clothing and contact a doctor.
If you suspect your child is playing with an asbestos-containing material, properly dispose of it immediately. Awareness and timely action can create a safer environment for your family.
Recommended Reading