Toronto Cancer Center Hosts SMARTEST Mesothelioma Clinical Trial
Research & Clinical TrialsWritten by Tim Povtak | Edited By Walter Pacheco

Princess Margaret Cancer Centre in Toronto recently opened a first-of-its-kind clinical trial that hopes to build on earlier pioneering efforts to turn pleural mesothelioma into a more manageable, potentially survivable disease. Expectations are high.
This single-center phase II clinical trial is named SMARTEST, and follows in the wake of earlier mesothelioma trials SMART and SMARTER in Toronto. SMARTEST is an acronym for Surgery for Mesothelioma After Radiation Therapy using Exquisite Systemic Therapy.
“The hope is that we find an effective therapy with little toxicity. That’s the dream for every cancer doctor,” radiation oncologist and principal investigator Dr. John Cho told The Mesothelioma Center at Asbestos.com. “At this point there is no cure, but being able to better control it, I can see that being a real possibility here.”
Clinical Trial Tests Radiation Before Surgery
The study involves an unconventional approach to this tough-to treat-cancer. It starts with low-dose radiation followed by low-dose cyclophosphamide, an older chemotherapy/immunosuppressive drug. Aggressive surgery is then performed, followed by the immunotherapy combination of tremelimumab and durvalumab.
“This is the latest, greatest version of our earlier SMART protocol,” Cho said. “We’re taking the next step.”
The study, which opened in May, is designed for previously untreated patients who qualify for aggressive surgery and are within mesothelioma stages 1-3. Estimated enrollment will be 30 patients.
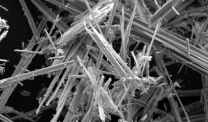
Pleural mesothelioma is typically caused by exposure to asbestos. It is usually treated with standard chemotherapy. Most patients survive less than a year.
The U.S. Food and Drug Administration recently approved the immunotherapy combination of nivolumab and ipilimumab, also known by the brand names Opdivo and Yervoy, for first-line treatment, but only a small percentage of patients have benefited significantly from the drugs alone.
Exploring Treatment Combinations Is Key
Most specialists agree that immunotherapy will be part of future mesothelioma treatment, but not alone, leading to a variety of studies to find a good match.
There are several other ongoing clinical trials involving immunotherapy drugs and a multimodality approach, but none to match the SMARTEST trials in Toronto.
For example, the Mayo Clinic in Rochester, Minnesota, opened a novel clinical trial recently to study the Opdivo/Yervoy combination when used alongside stereotactic body radiation therapy.
Memorial Sloan Kettering Cancer Center in New York City has one clinical trial studying Opdivo and standard chemotherapy before surgery for mesothelioma, and another using intensity-modulated radiation therapy and chemotherapy after surgery.
In the earlier SMART trial, a cohort of 19 mesothelioma patients with the epithelial cell type and no lymph node involvement produced a median survival of 5.5 years, the first time a multimodality study for mesothelioma exceeded the five-year mark.
When all 96 patients in the study were included, the median survival dropped to 24.4 months with a disease-free survival of 18 months.
The SMART trial involved a higher radiation dose before extrapleural pneumonectomy surgery, which removed the entire diseased lung, but did not include immunotherapy drugs afterward.
Radiation Can Stimulate Immune System
The theory behind using the unconventional radiation-first, higher-dose procedure is that it can better stimulate the immune system, which decreases the cancer’s ability to spill, or seed, in the chest cavity during surgery. This can reduce mesothelioma recurrence.
Toronto’s SMARTER trial involved a lower dosage of radiation and the lung-sparing pleurectomy and decortication surgery, which results in a much shorter recovery time for patients. It also used no immunotherapy drugs after surgery.
SMARTER, or Surgery for Mesothelioma After Radiation Therapy using Extensive Resection, allowed for a wider range of patients, admitting those who couldn’t tolerate the lung-removing surgery.
Although final results of SMARTER have not been released, they are not expected to reach the lofty median survival times of the SMART trial.
SMARTEST also will be using the lung-sparing surgery and lower dose radiation, but with the cyclophosphamide before surgery and the immunotherapy combination afterward, which is expected to extend survival without adding toxicity.
“We wanted to design a study that had the same advantages of the SMART trial, but without the tough recovery period, less toxic and with fewer side effects,” Cho said. “I think your own immune system can fit that need, almost like the proverbial magic bullet.”