The Future of Cancer Treatment: Using Technology to Find a Cure

Written by Sean Marchese, MS, RN | Edited By Walter Pacheco

Cancer remains the illness most feared in the United States. Most Americans say cancer technology advancements are key to lowering incidence rates, improving life expectancy, and bringing us closer to a cure for cancer.
That’s why innovative approaches to molecular biology, such as gene-editing tools and nanomedicine, could play a role in the future of cancer treatment. Breakthroughs in computer science, including artificial intelligence and virtual reality, may also spur new cancer treatment.
Who benefits from the latest cancer research? Patients and their loved ones. These new technologies and advances in cancer treatment could revolutionize the way we treat the disease, from earlier cancer detection to improved quality of life for all cancer patients.
“I believe with the forward direction technology and computers are heading, computer advancement could definitely make a great impact on cancer care,” peritoneal mesothelioma survivor Tamron Little said. “It will take a lot of research to develop more specialized treatments that target the cancer without many harmful side effects.”
Cancer Treatment Timeline
-
2022
Next Generation of mRNA Cancer Vaccines

-
2021
Molecular Profiling
-
2017
FDA Approves First Cancer Gene Therapy
-
2014
Analysis of DNA in Cancer

-
2011
Tumor Treating Fields

-
2001
DaVinci Surgery System for Cancer

-
1990s
CAR-T Cell Trials Begin in Humans

-
1986
FDA Approves Alfa-Interferon
-
1953
Chemotherapy Cures Solid Tumor
-
1890s
Development of First X-Ray

How Is Computer Science Shaping the Future of Cancer Treatment?
Computer science uses hardware, software, algorithms and data collection to shape how researchers and oncologists develop the most personalized and effective cancer treatment.
Robotic-assisted surgery, which is a technology with growing potential, is the most tangible example of computer science working to treat cancer with greater precision than traditional surgical procedures.
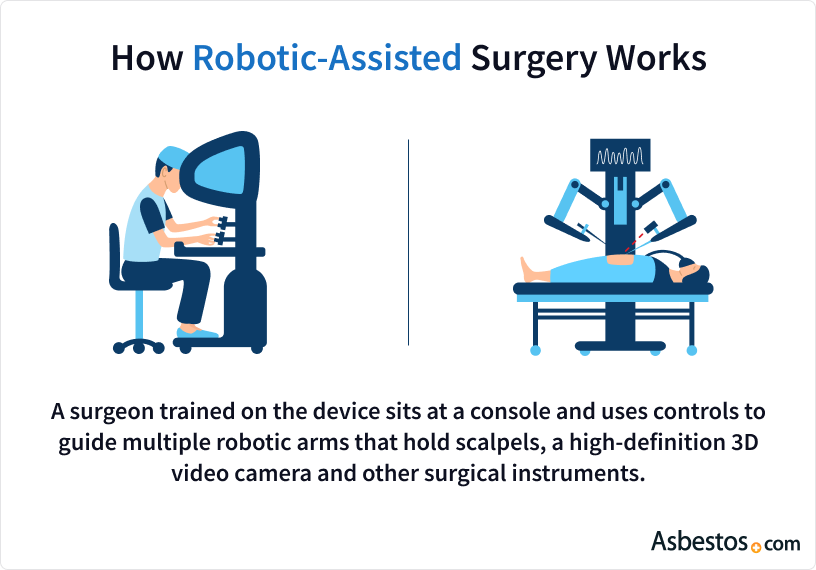
How Does Robotic-Assisted Surgery Work?
A surgeon trained on the device sits at a console and uses controls to guide multiple robotic arms that hold scalpels, a high-definition 3D video camera and other surgical instruments.
In 2021, several U.S. cancer centers, including University Hospitals in Cleveland, started using the Monarch Platform. This device is another robotic-assisted tool that obtains biopsies from hard-to-reach nodules deep in patients’ lungs.
The goal of this type of robotic surgery: Earlier lung cancer diagnoses can lead to earlier treatments and improved long-term results for cancer patients.
The Monarch Platform builds upon robotic treatment technology started by the da Vinci surgical system, which was first used in cancer treatment in 2001.
Computer technology has massive potential for the future of cancer treatment, especially in the evolving fields of artificial intelligence, virtual reality, implantable sensors and other technologies.
Could AI Lead to Cancer Breakthrough?
Cancer researchers are making strides using artificial intelligence, also known as AI, in the early diagnosis of cancers, development of new cancer treatment and preventing cancer tumor growth.
Artificial intelligence is a computer software that relies on a series of instructions to accomplish a useful task. These instructions are called algorithms that function like directions in a pie recipe.
Researchers at Case Western Reserve University and Cleveland Clinic, among other Ohio cancer centers, ran a limited study in 2020 to see if AI could determine whether immunotherapy promoted cancer growth in a small subset of lung cancer patients.
The results showed that using AI to analyze CT scans of tissue identified biomarkers that could show which of the 109 non-small cell lung cancer patients in the study would experience tumor growth from immunotherapy.
In 5 to 10 years’ time, I hope we will see personalised immunotherapy. This means that doctors – probably through a computerised AI algorithm – would be able to incorporate information about the individual, their tumour, their immune system, and their genetics to create a personalised prescription for the type of immunotherapy or combinations that would be most likely to work for that person.
Researchers will use that technology to teach computers to make AI better at detecting cancer and other diseases.
AI could improve the medical scan image quality of MRI and CT machines. It would also reduce patients’ radiation exposure by increasing the scan’s precision. Researchers developed one of the earliest AI programs in 1965, named DENDRAL, and it helped chemists discover unknown forms of medications.
Another advantage: AI will be a more cost-effective alternative for drug discovery and development. AI programs can check for new uses of existing medications and reduce the burden on expensive clinical research.
Advances in Cancer Research with Virtual Reality
While virtual reality for cancer patients has not advanced to the level of a potentially curative treatment, it has shown progress in cancer symptom management.
Virtual reality, also known as VR, lets patients interact with a simulated environment through special goggles. The device replaces the user’s sight with an imaginary scene.
Some simulations feature relaxing environments such as a beach with the sound of waves and birds. Others may provide educational scenes that show how a cancer patient is diagnosed.
A study published in the Journal of Cellular Physiology in 2020 showed that breast cancer patients using VR while undergoing chemotherapy showed improvements in their moods.
The patients were immersed in scenes involving animals and nature, according to the study. These women showed less anxiety, depression and fatigue than the other women who were not exposed to virtual reality during therapy.
Researchers say those types of results show VR can lead to improved psychological support for cancer patients as a palliative treatment, and that could translate to better survival and quality of life.
Moffitt Cancer Center in Tampa also partnered with Ringling College of Art and Design in 2020 to create a VR program to help reduce stress in cancer patients, connect them to survivor stories and help them better understand their cancer treatment.
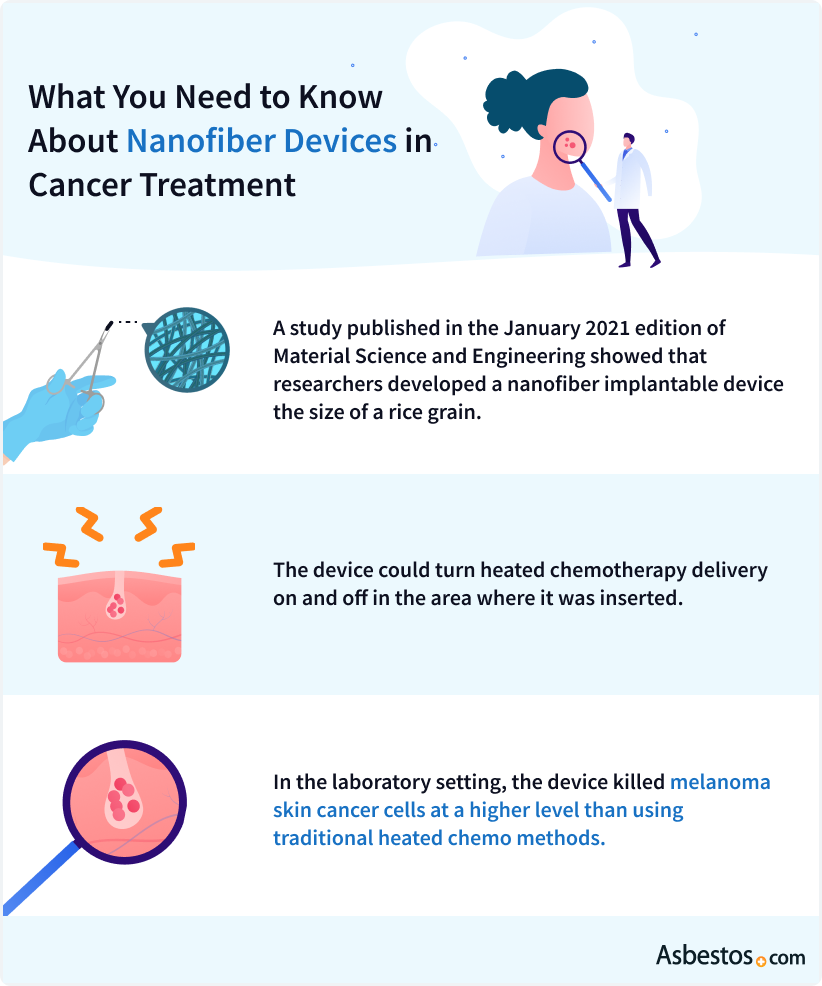
Using Nanotechnology as New Cancer Treatment
The role of nanotechnology in cancer care has focused mostly on using implantable sensors that deliver anticancer medication with greater precision than traditional methods.
Nanotechnology involves the design, production and application of incredibly small devices and systems. These devices are generally between one and 900 nanometers in length.
Visualizing how tiny that can be is nearly impossible. But for comparison, a human fingernail grows one nanometer per second. And a human hair is about 100,000 nanometers wide.
In 2022, a research team at the National Cancer Institute published their work on an innovative therapy for pleural mesothelioma using a spray-on hydrogel during surgery. The new treatment involves spraying genetically engineered nanoparticles on the cancer site to eliminate mesothelioma tumor cells left behind after surgery.
A February 2021 research study published in Emergent Materials proposed using nano-based antimicrobial technology in personal equipment to protect health care workers from viral diseases such as COVID-19.
Another team of researchers in 2020 developed a mint-sized device to regionally deliver cisplatin, a common chemotherapy drug. The lab study found the device’s delivery of cisplatin was “significantly toxic” to breast and liver cancer cells.
At Memorial Sloan Kettering Cancer Center, researchers in 2019 began developing a biosensor that can be implanted in the uteruses of women at high risk of ovarian cancer.
The intrauterine device will quickly alert doctors if it detects elevated, local levels of ovarian cancer biomarkers. If development of the device is successful, it could improve early-stage diagnosis and lead to more personalized treatments.
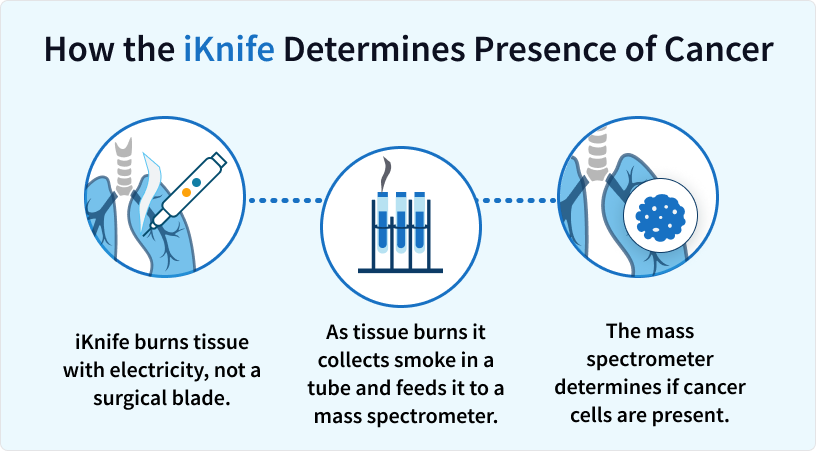
iKnife: New Cancer Fighting Technology Using Smoke
A device called an intelligent knife, also known as an iKnife, burns tissue with electricity, not a surgical blade. As the tissue burns, the iKnife collects the smoke in a tube and feeds it into an advanced computer called a mass spectrometer. That machine determines if cancer molecules are present.
A 2021 breast cancer clinical trial at Imperial College Healthcare in the UK is one of the first human trials with iKnife. A separate 2021 study in the journal Analytical Chemistry validated the iKnife’s ability to differentiate tissue on par with laboratory examination.
The iKnife presents several benefits. For example, the device detects cancer molecules closer to real time instead of the days or weeks it takes for a pathologist to receive and analyze a biopsy. Doctors use tissue or cell samples taken from biopsies to learn disease information, such as cancer type.
Thanks to the near immediate analysis of cancer tissue, surgeons know whether they are cutting healthy or cancerous tissue during the surgery. This information produces a clear tumor outline in the operating room and could decrease the rate of repeat surgeries or cancer recurrence.
The iKnife can also detect the types of fat that tumors use for growth, alerting cancer patients to which fats they should avoid in their diet.
Tumor Treating Fields: New Technology for Cancer Treatment
Tumor treating fields, also known as Optune or TTFields, is an evolving new cancer technology developed for treating cancer with electric fields.
TTFields are administered using a portable, lightweight device. Four adhesive patches attached to the machine are placed on the area of the body near the cancer.
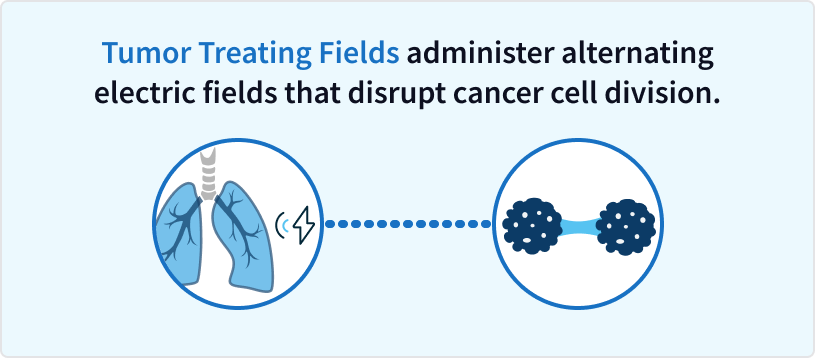
The patches then deliver low intensity, alternating electric fields to that region. The electric fields disrupt tumor cell division.
A clinical trial expected to end in 2026, dubbed TRIDENT, is studying the potential survival benefit of using tumor treating fields alongside radiation therapy and a chemotherapy drug.
TRIDENT is currently enrolling brain cancer patients at the Mayo Clinic in Arizona, H. Lee Moffitt Cancer Center and Research Institute in Tampa, Advent Health in Orlando and other cancer treatment centers in the U.S.
Tumor treating fields in 2019 received FDA approval for the treatment of mesothelioma.
The success of the latest clinical trial using tumor treating fields could shape the future of cancer treatment for patients with rare or aggressive malignancies such as glioblastoma multiforme (GBM). GBM accounts for 46% of primary brain cancers, and overall patient survival is approximately 14 months.
Developing Cancer Technology Advancements Using Cancer Biology
Cancer biology, and more specifically, molecular biology, is an area where technology in cancer care and research may lead to a new cancer treatment breakthrough.
Molecular biology is the study of cells and the building blocks of life, including DNA. Biologists have learned how to break down these molecules and rebuild them for new purposes such as gene-editing tools that manipulate the DNA of tumor cells to make them less resistant to anticancer medications.
There’s also ongoing research on how to use exosomes, which are tiny cells that carry proteins and genetic information between cells, as a Trojan horse to deliver anticancer medicine to tumors.
While these advances in cancer treatment are not as easy to visualize as an implantable sensor or robotic surgical arms, scientists are hopeful their work can lead to a new cancer treatment or a cure for cancer.
Cancer Technology Advancements Using CRISPR
CRISPR, pronounced “crisper,” is a new cancer technology and gene-editing tool that works like a pair of scissors and glue for making repairs to DNA. Cuts in DNA can disable certain genes, remove cancer mutations or fix a production problem.
In February 2021, drugmaker AbbVie and Caribou Biosciences announced both will use CRISPR to improve CAR T-cell therapy, which genetically engineers a patient’s T-cells (type of white blood cell) to fight cancer.
As a possible new technology for cancer treatment, gene editing with CRISPR takes months, not a year or two, to genetically modify T cells. That may mean much faster treatment for patients.
The potential for genetic medicine is groundbreaking. Altering parts of DNA can redefine how your body fights off cancer. This technology can provide hope for patients by improving treatment specificity and reducing the risk of cancer recurrence.
Scientists can cut drug-resistance genes out of cancer DNA. The result would mean more effective chemotherapy that can stop mutations from developing into aggressive malignancies and a better quality of life for cancer patients.
Doctors could also use CRISPR to screen patients for high-risk DNA mutations and edit out the cancer-causing gene.
The first cancer clinical trials using CRISPR began in 2019. They focused on improving existing lung cancer treatments such as chemotherapy.
New Nanomedicine Techniques for Treating Cancer
Nanomedicine is the medical practice of using small, human-made particles to treat disease. These tiny particles work like building blocks or construction materials. Scientists can arrange them into different shapes, such as boxes or long tubes, to interact with tumor cells.
In September 2020, researchers at the University of Illinois discovered a new method of forming gold nanoparticles within cells. The new technology is impressive because it minimizes toxicity to healthy cells. Gold is generally safe and nonreactive within the body, but when heat-activated, it can destroy tumors.
Gold nanoparticle therapy targets tumors at a molecular level and reduces the chance of damaging healthy cells compared to chemotherapy. Patients who receive this type of nanomedicine could improve their prognosis without severe side effects.
Nanotechnology is the science of building microscopic structures, such as long tubes, out of molecules, and nanomedicine applies that technology for patient care. A recent study from January 2021 published its results on carbon nanotubes combined with immunotherapy for breast cancer treatment; patient survival increased by 55%.
About 287,850 new cases of invasive breast cancer will be diagnosed in women in 2022. In a 2022 survey by The Mesothelioma Center, 74% of women agree that more research on cancer technology is needed to adequately treat cancer.
Cancer Technology Using Exosomes for New Treatments
Molecular biologists are finding novel uses for exosomes, a method that cells use to communicate. Exosomes are tiny bubbles of cellular matter that enter and exit cells to send information or particles.
Exosomes are about 30 to 100 nanometers in size and play crucial roles in body function, such as the regeneration of injured tissue. Exogenous Therapeutics developed a form of inhaled exosomes that could repair lung tissue damaged by COVID-19.
The technology involves reprogramming exosomes to deliver medication right to a tumor site. A January 2021 study published in the journal Biomaterials describes how researchers use exosomes to improve immunotherapy effectiveness.
Scientists in the study constructed exosomes that could deliver cancer medication into tumors and simultaneously make tumors more vulnerable to an immune response. This new combination of exosome technology and medication delivery increases the drug accumulation within tumors while also signaling the immune system to attack cancer.
A January 2021 report describes cisplatin-loaded exosomes that can prolong the survival of mice with ovarian cancer. The exosome-loading technology avoids any liver or kidney side effects, unlike cisplatin used alone. With fewer side effects, patients could stay on cancer treatment longer.
Exosomes solve some other common problems with existing cancer treatment. For example, in November 2020, researchers at the University of Kansas detailed the benefits of exosomes small enough to cross the blood-brain barrier. This advantage could help improve existing brain cancer medication.
Improving Diagnostic Testing with New Cancer Technology
A new type of diagnostic technology helps doctors diagnose cancer by looking for circulating tumor DNA or “ctDNA.” Cancer grows and replicates at a rapid pace. As some of those cells die, they release their DNA and other contents into the blood.
New testing technology can detect ctDNA in the blood before any growths or masses show up on imaging, leading to an earlier diagnosis. For the patient, identifying ctDNA only requires a blood test. With the results, doctors can assess tumor cell type and genetic makeup, which usually requires an invasive surgical tissue biopsy.
Cell type is everything. This is more important than stage, in my opinion, since it can help predict outcome and guide treatment options.Dr. Raja FloresChairman of the Department of Thoracic Surgery for the Mount Sinai Medical Center in New York City.
A research team in China published their work in March 2021 on a supersensitive silicon nanowire array biosensor. This latest sensor can detect cancer DNA at lower levels than ever before. With an earlier cancer diagnosis, patients have access to more treatments and a better prognosis.
Researchers in Australia shared their research on a new bladder cancer-detecting device in a January 2021 paper in Biosensors and Bioelectronics. The new device uses fluorescence to detect bladder cancer cells in urine with nearly 100% accuracy. The technology could remove the need for invasive biopsies.
Improving Diagnostic Testing with New Cancer Technology
Doctors often use predictive models to make pre-clinical decisions about a patient’s treatment plan. For example, scientists can take a portion of the patient’s tumor tissue, implant it into a laboratory mouse, and study its reaction to various therapies. That information helps doctors choose the best methods for cancer treatment.
This type of predictive model is called a patient-derived xenograft, and clinical researchers have been improving the technology behind accurately predicting a patient’s treatment response.
A February 2021 study examined the benefits of using zebrafish instead of mice to model human tumors and found an 82% match for human disease genes. In a paper published in January 2021 in Cancer Chemotherapy and Pharmacology, scientists outline how zebrafish xenografts have led to drug discoveries for prostate cancer.
Predictive model technology may soon advance beyond the need for genetically similar animals. A newer process called in silico modeling uses computers instead of living tissue to run virtual tests and simulations. In March 2021, a research team used in silico trials to develop potential vaccines against lung cancer-causing viruses.
Doctors may develop better treatment plans for their patients, and scientists could create new and better drugs to fight cancer using predictive model technology. With additional research and funding, future advancements in cancer biology could lead to a potential cure.
What Do People Say About Funding the Future of Cancer Treatment?
In February 2022, The Mesothelioma Center at Asbestos.com conducted multiple surveys of nearly 1,000 Americans to gauge the public’s support for future cancer treatments and the funding to pay for the research and development of new cancer technology.
The results show most people believe there is an opportunity to improve cancer care technology.
Do We Need More Cancer Research?
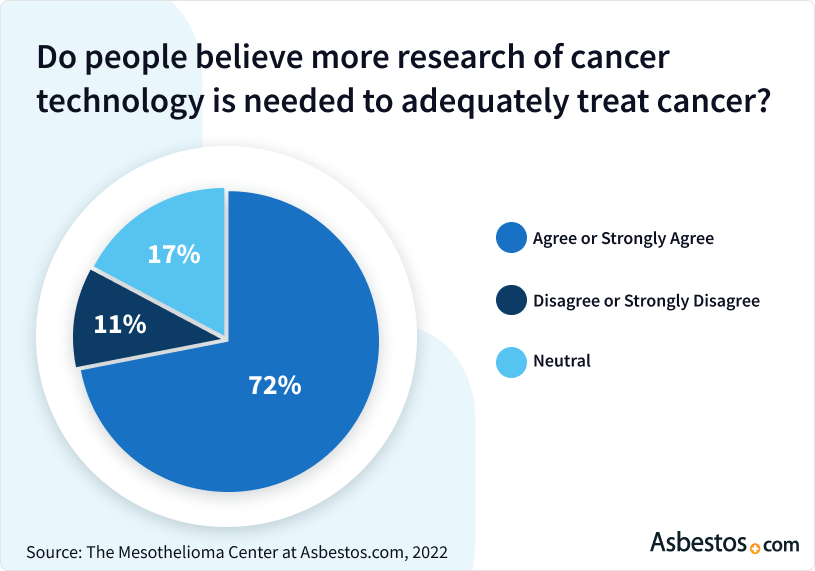
Cancer patients, especially those in the late stages of the disease, often feel as though they don’t have enough options for treatment. A financial investment in cancer research would likely increase treatment choices and availability.
Unfortunately, most Americans are unwilling to personally donate and fund new cancer research initiatives.
Are Americans Willing to Donate to Cancer Research?
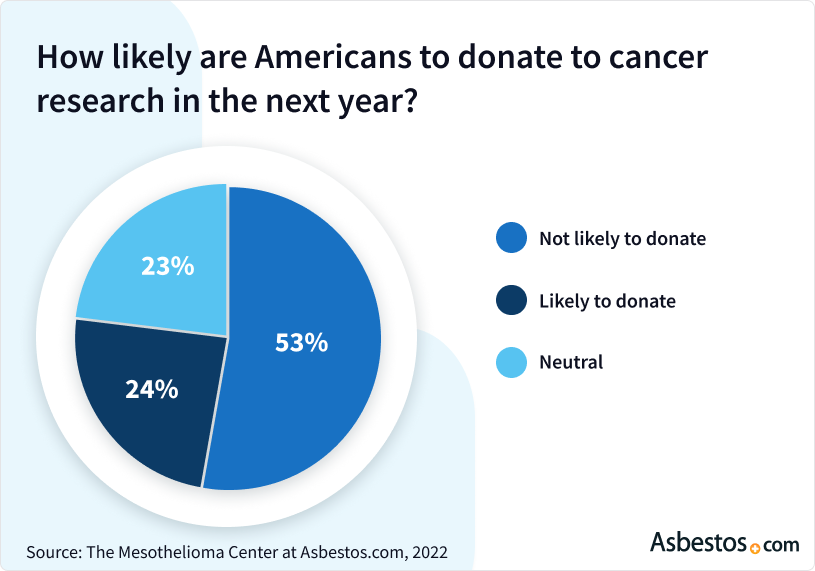
Public and government values may align with a desire to reduce cancer deaths through research into better technologies, but it’s clear that funding cancer research faces obstacles.
Evidence shows public opinion supports the need to further cancer research, which aligns with recent government initiatives. In February 2022, the Biden administration announced a relaunch of the Cancer Moonshot initiative to cut cancer death rates in half by 2047.
How Age Impacts Response to Funding Cancer Research
When responders were asked if they thought more research on cancer technology was needed to treat cancer adequately, older adults agreed the strongest.
About 64% of respondents aged 55 to 64 stated they strongly agreed with the need for more cancer research, followed by nearly 58% of respondents aged 45 to 54.
Cancer will most likely affect older adults. In 2022, the American Cancer Society reported that they expect more than 1.7 million new cancer cases for both men and women age 50 and older.
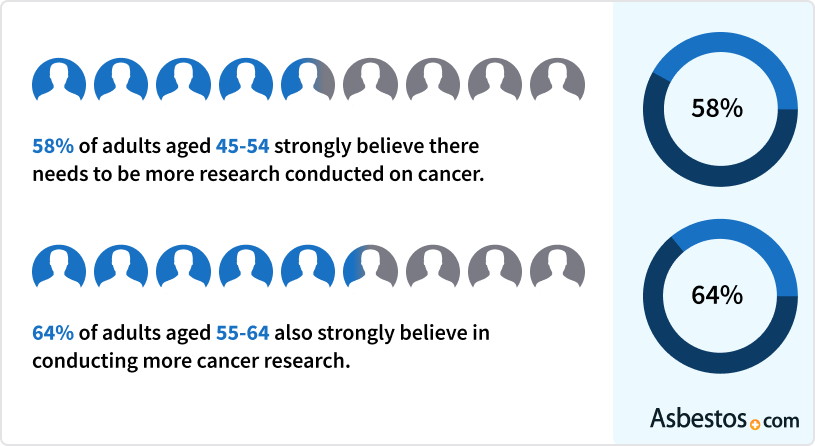
The survey showed 7% of respondents aged 35 to 44 strongly disagreed with the need for more research, the highest percentage of any age group. A total of 43% of the same age group also said it was not likely they would donate to cancer research in the next year.
Young people were the most willing to donate. A total of 23% of respondents between the ages of 18 and 24 said they were very likely to contribute funds to cancer research over the next year. People in this age range may see cancer research as an investment in their future more than conservative older adults.
How Gender Influences Response to Funding Cancer Research
Men are slightly more likely to develop cancer over the next year, according to the American Cancer Society’s 2022 Surveillance Research. They predict 983,160 new cancer cases for men and 934,870 for women.
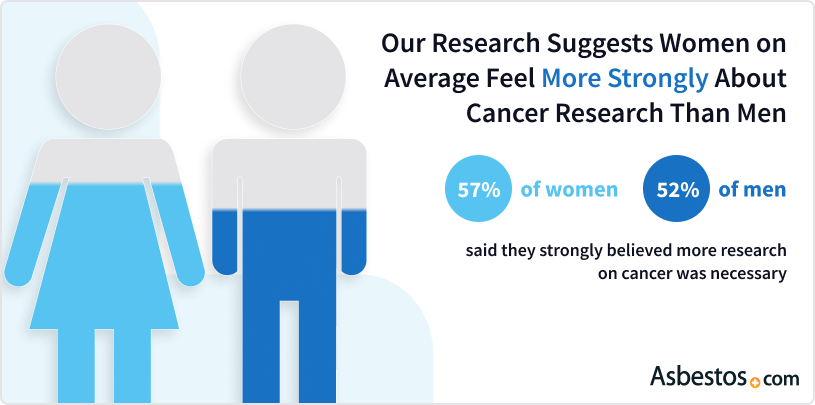
The median age of breast cancer diagnosis is 62. Breast cancer primarily affects women ages 50 and older, explaining the higher interest in cancer research within this demographic.
However, both women and men were equally doubtful they would personally help fund cancer research. Only about 12% in each group said a personal donation was very likely.
Adults aged 65 and older had the most significant discrepancy by gender when deciding whether they would donate to cancer research in the next year.
In that age group, the survey showed 40% of women and 53% of men said it was “very unlikely” they would donate to cancer research in the next year, while 16% of women and 8% of men said it was “very likely” they would.
Making Future Cancer Treatments a Reality
It’s no secret that the largest barrier to technology in cancer research and treatment is funding. Developing a cancer breakthrough is expensive. Clinical research trials need experienced personnel and enough resources to guarantee patient safety.
However, new cancer technologies are necessary steps toward a future without cancer. Thankfully, the science behind today’s cancer technology advancements continues to improve every day.
What specialists think of as the standard of care today will likely look much different within the next 20 years.
New technologies are created by humans, so they are subject to the same human errors and biases. But with continued study, refinements and adjustments, they can greatly improve the delivery of care.Dr. Raja FloresChairman of the Department of Thoracic Surgery for the Mount Sinai Medical Center in New York City.
Patients can help with this initiative by registering for clinical trials. One of the biggest failures of clinical research is low patient enrollment. Patients who ask their health care team about clinical trials often find resources they never knew existed.
There’s no limit to what we can achieve with a dedication to science and research. Thanks to a bright future for cancer treatment technology and the advances in cancer treatment, there is great potential for more researchers to find a cure for cancer.



