38 Hospice Facts, Statistics and FAQ
Written by Amy Pelegrin | Edited By Walter Pacheco
The number of Americans using hospice services is rising as the proportion of the population over 65 increases faster than ever before. According to the National Hospice and Palliative Care Organization, over 1.6 million Medicare beneficiaries are enrolled in hospice care.
But what exactly is hospice? While seven out of 10 Americans say they know a little bit about hospice, not everyone is aware of this type of care and the benefits it can bring to patients and their families. As a medical care path with a goal to relieve suffering, it is often confused with palliative and comfort care due to similarities. The main differences are:
- Hospice care is a team approach to medical care aimed to optimize a patient’s quality of life once treatment is no longer of benefit or when a cure is no longer feasible. When a doctor estimates a patient has less than six months to live, the patient can enroll in the Medicare hospice benefit. All of the patient’s medications, necessary services and equipment are provided through hospice at little to no cost through Medicare or private insurance.
- Palliative care also strives to improve the quality of life of patients living with a serious illness at any stage of their medical journey. It is often combined with a treatment plan incorporating curative or therapeutic care.
- Comfort care is one part of hospice care, which reduces the intensity of medical care and focuses on improving a patient’s quality of life when they are nearing the end of their life.
- Respite care is defined as temporary patient care in a facility that allows a primary unpaid caregiver (such as a spouse, child or friend) to take a break from constant caregiving and rest for up to five days.
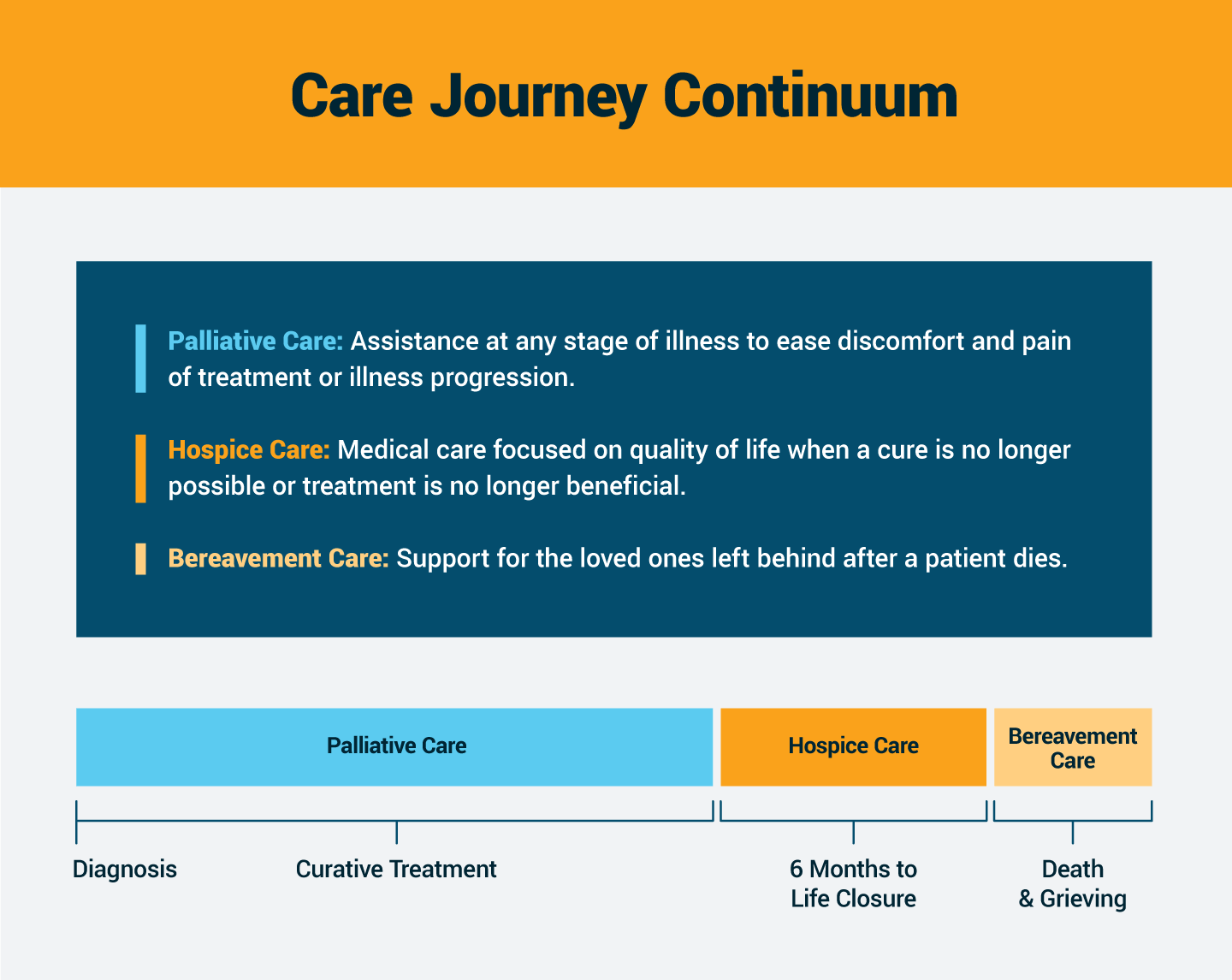
One key element of hospice care is the interdisciplinary combination of doctors, nurses, pain management specialists, and emotional and spiritual support. Each patient’s hospice team tailors the care plans to the wishes and needs of the individual patient and their family. The focus becomes caring instead of curing at this stage. Hospice even includes bereavement care for the patient’s family members after their death.
To help both inform the general public and dispel common misconceptions about hospice in America, we outline important facts and statistics below.
Average Hospice Length of Stay and Other Key Statistics
The time a person stays in hospice varies from patient to patient. Hospice care needs are different for everyone, so two patients with the same illness may stay in hospice for drastically different lengths of time.
-
On average, Medicare patients remain in hospice for 92.6 days during their lifetime.
-
In 2019, 1.61 million Medicare beneficiaries were in hospice for a total of 121.8 million days of care.
-
51.6% of people who died while on Medicare in 2019 were enrolled in hospice at their time of death.
-
76% of hospice centers admit patients within 4 hours of the initial hospice referral from the patient’s doctor.
-
The 5 most common principal diagnoses for patients in hospice are (in order of prevalence):
- Dementia, including Alzheimer’s and Parkinson’s
- Respiratory Illness
- Circulatory/Heart Illness
- Stroke
- Cancer
-
Only 1 in 3 Black Medicare participants signs up for hospice care, compared to almost 50% of white beneficiaries.
-
Women are more likely to utilize hospice than men. 56.2% of the female-identified Medicare beneficiaries who died in 2019 were in hospice, compared to only 46.7% of those who were male-identified.
-
Death is not a guaranteed outcome of hospice, as 17.4% of Medicare participants enrolled in hospice were discharged alive in 2019.
How Expensive Is Hospice and Who Covers the Costs?
Medicare covers the majority of costs associated with hospice. But there are certain elements that may partially be the patient’s financial responsibility, including prescription copays and inpatient respite care.
-
Hospice is the least expensive health care environment for patients, with an average cost of $190 per day for routine home care.
-
There are four levels of care covered fully or at least partially by Medicare hospice benefits:
- Routine Home Care
- Continuous Home Care
- Inpatient Respite Care
- General Inpatient Care
-
Medicare paid U.S. hospice providers almost $21 billion for care services in 2019.
-
The overwhelming majority of Medicare spending for hospice expenses is for routine home care.
-
Similar to Medicare’s hospice benefit, U.S. military personnel and their families can access hospice coverage through TRICARE.
-
Medicare paid more than $6.6 billion over a 10-year period to nonhospice providers for items and services.
-
To adhere to the Medicare Conditions of Participation (CoPs), hospice centers are required to use volunteers for at least 5% of patient care.
Common Hospice Myths and Misconceptions
The public is generally poorly educated on the concept of hospice care, resulting in a wide variety of myths to develop and flourish. Those with a stronger understanding of hospice tend to appreciate its benefits. One recent survey revealed that 42% of home health agency leaders believe the public has a positive perspective on home health.
-
Myth: Only people on the verge of death should be in hospice.
Truth: Patients can access hospice care up to 6 months prior to their projected death. Studies have revealed that some hospice patients live longer than patients with the same illness who are not in hospice.
-
Myth: Hospice care ends when a patient dies.
Truth: Many hospice care services include bereavement care and grief support for the family members left behind.
-
Myth: Once you enter hospice care, there is no turning back.
Truth: Patients are free to withdraw from the hospice program at any time without penalty. They retain the option to re-enroll as long as they still meet the medical eligibility requirements.
-
Myth: People who are dying must leave their homes for hospice care.
Truth: The majority of hospice patients opt to receive care in their own residences, whether they be private homes, long-term care facilities or assisted living communities.
-
Myth: Hospice is meant only for cancer patients.
Truth: Hospice care began in the United States in the 1970s and focused primarily on assisting terminal cancer patients. Now hospice is used by patients with a broad range of diagnoses. As of 2021, patients with Alzheimer’s and dementia accounted for the largest portion of hospice care patients by far.
-
Myth: Hospice care is expensive.
Truth: Medicare’s hospice benefits are fully funded and cover the majority of costs faced by beneficiaries, making hospice one of the least expensive care plans available to patients. Most private insurance also covers hospice expenses.
-
Myth: Hospice is only for elderly adults.
Truth: Any person who meets the eligibility guidelines — no matter their age — can enroll in hospice care.
Hospice Care Industry
There were over 4,800 Medicare-certified hospices in business in 2019, when the last count was published. That total represents an increase of more than 18% since 2014. The type of care available also continues to expand, with many hospices now incorporating pediatric care and concierge services.
-
The American hospice industry was valued at $32.1 billion in 2021 and is estimated to reach $64.7 billion in revenue by 2030.
-
The national health care staffing shortage has had a negative impact on 98% of hospice organizations.
-
Approximately 71% of hospice centers are for-profit, 26% are nonprofit and 3% are government-owned.
-
Nurses are leaving or considering leaving hospice and other health care jobs due to:
- Burnout
- Poor staffing
- Stressful working environments
Home, Health and Hospice Study
-
Almost 80% of hospice facilities state that at least 20% of their current job openings for nurses remain unfilled.
Home, Health and Hospice Study
-
Home health aides have the highest job turnover rate of all home-based health care jobs, at 36.53%.
-
Case managers at the top-performing home health centers average caseloads of 20-25 patients.
-
Since 2021, 72% of hospice centers have been forced to turn away patient referrals due to the national staffing shortage.
Home, Health and Hospice Study
History of Hospice and Palliative Care
The concept of hospice first evolved in England in the middle of the 20th century, when it was innovative to focus on the quality of life for dying patients. In the decades since, it has spread across the world and become a valued asset in modern health care.
-
1967: Dame Cicely Saunders revolutionized health care by opening the first modern hospice outside of London after she recognized that the quality of life for terminal patients improved when they were removed from sterile hospital environments.
-
1974: Florence Wald, former dean of the Yale School of Nursing, co-founded the first hospice in the U.S. called Connecticut Hospice in Branford, Connecticut.
-
1978: The National Hospice Organization (NHO) was established in an effort to promote the concept of hospice care across the United States.
-
1982: Medicare hospice benefits were established under the Tax Equity and Fiscal Responsibility Act of 1982, covering care for 80%-85% of hospice beneficiaries.
-
1988: The Community Health Accreditation Program (CHAP) for accrediting hospice care centers began.
-
1991: A veterans health care commission recommended adding hospice to the veterans benefits package.
-
2000 to Today: As awareness of hospice options have grown, a study of Medicare beneficiary deaths since 2000 revealed an increase in patients dying in their homes or community health care facilities and a decrease in hospital deaths.
-
2004: Hospice care in the U.S. achieved a major milestone for the first time, serving over 1 million people with a life-limiting illness.
Hospice FAQs
When surveyed, 71% of Americans feel that “helping people die without pain, discomfort and stress” is the most important aspect of end-of-life healthcare. Identifying how best to support a dying loved one in achieving that can be daunting. Some questions about hospice repeatedly pop up as people strive to both understand and make the most of hospice services.
What’s Included in Hospice Care?
A broad spectrum of services and equipment are available in hospice care. They may include:
- Medical management of a patient’s pain and other symptoms
- Medications, medical supplies and equipment for pain relief and symptom management
- Physical, occupational and speech therapy services
- Home aide services
- Nutritional/dietary counseling
- Short-term inpatient care
- Inpatient respite care
- Spiritual and/or grief counseling for both the patient and surviving family members
Where Do Patients Receive Hospice Care?
Considering that 71% of Americans would prefer to die in the comfort of their own home, it makes sense that most hospice care services are provided in the patient’s home. For these services, “home” may be interpreted as a private residence, a nursing home or other residential facilities. By establishing care within the home, family members are typically able to serve as the primary caregiver for the patient. The hospice care team makes regular visits to the home to gauge the patient’s health status and provide any additional care needed. In a recent survey of hospice health agencies, 92% noted that they also use telehealth as an additional option for receiving care.
Can I Keep My Doctor Once in Hospice?
A patient’s existing doctor or specialist is strongly encouraged to continue participating in their care. The hospice physician consults with the family physician since they usually know the patient’s medical history best. They may also confer while developing the patient’s care plan to identify any unique medical needs of that patient.
Does Hospice Provide 24/7 Care?
Yes and no. Hospice staff are on-call at all times, 24 hours a day, seven days a week. But hospice personnel will not be present at a patient’s bedside around the clock. They are often juggling over 20 cases at a time and cannot dedicate 24 hours to one patient’s care.
Will I Have to Stop Other Medications If I’m in Hospice?
In order to begin hospice, a patient must cease all curative medication and treatments being used to control their illness. But patients are permitted to remain on medications that treat other conditions or symptoms.
Should I Add Hospice Care to my Advanced Care Directive?
Yes, planning ahead for your future health needs is important to ensure that you receive care aligned with your wishes. Incorporate those decisions into an Advanced Care Directive and other end-of-life documentation. Research has shown that patients who have taken the time for advanced care planning are usually more satisfied with the care they receive.
2022 marks the 40th anniversary of the passage of the Medicare hospice benefit legislation. One Kaiser Family Foundation study tells us that, among Americans who have recently lost a loved one, 53% say that the person received hospice care services prior to their death. As the visibility of hospice care and its benefits increases, the services it encompasses will continue to assist millions of people for years to come.
Find hospice care services near you through the Medicare website.






