
Connect with top-rated mesothelioma specialists at a cancer center near you, who will personalize treatment options based on your diagnosis.
Find Your CenterA mesothelioma blood test checks for specific proteins (biomarkers) linked to the cancer. These include n-ERC mesothelin and fibulin-3. Doctors use blood tests and biopsies to help diagnose mesothelioma. MESOMARK is the only blood test approved by the FDA for mesothelioma detection.
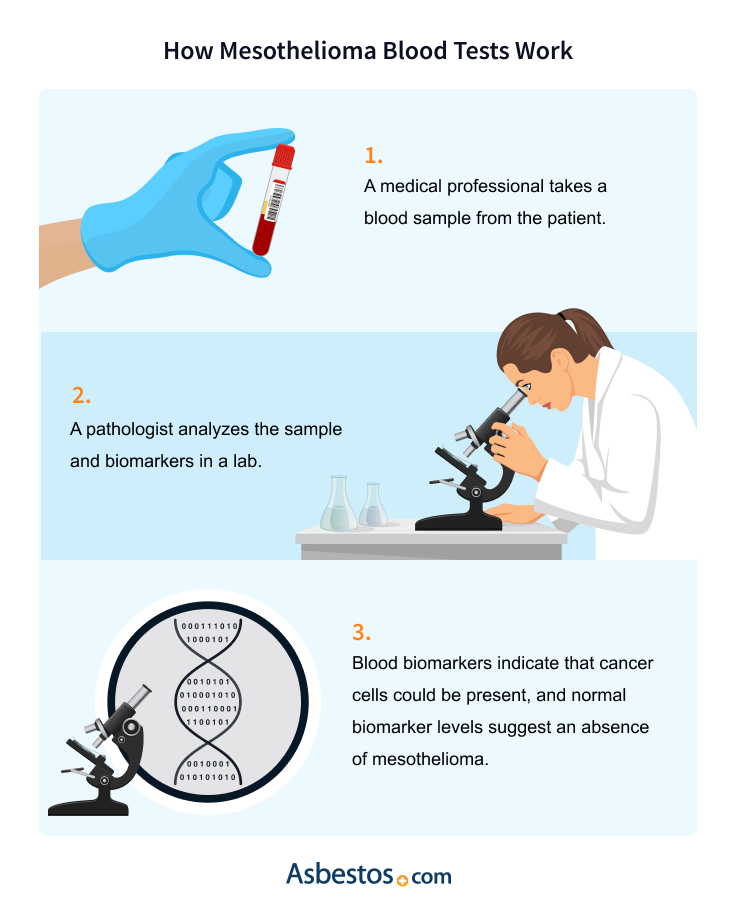
Mesothelioma blood tests are procedures that use a small sample of your blood to check for signs of this rare cancer. During these procedures, a health care provider takes blood from your arm. A pathologist studies your blood in a laboratory for certain proteins and other changes that may appear if you have mesothelioma.
Doctors use these blood tests as a tool to learn more about your health. Results can help decide if you need more testing, help track your overall health or show how your body is responding to treatment. These tests support your care but don’t diagnose mesothelioma on their own.
No blood test can detect asbestos exposure. Biopsy tests of tissues can reveal the presence of asbestos fibers that can get stuck in tissues. Doctors often use biopsies to determine a diagnosis of mesothelioma.
Mesothelioma blood tests look for proteins in your blood that may be linked to this cancer. Patient Advocate Snehal Smart, MD of The Mesothelioma Center tells us, “There are no biomarkers specific to mesothelioma.” But some proteins like calretinin, WT-1 and mesothelin often appear at higher levels in people with mesothelioma.
One test called MESOMARK checks for specific protein molecules called soluble mesothelin-related peptides. Snehal says SMRP is “usually high in patients with mesothelioma.” She explains that while the test alone can’t confirm the disease, “high levels of the SMRP protein can indicate a probable diagnosis of mesothelioma.”
These blood tests can help doctors rule out other cancers or spot signs of mesothelioma early. You’ll still need other tests like biopsies and imaging scans for a mesothelioma diagnosis. Blood tests are just one part of the process doctors use to diagnose this disease.
The most common mesothelioma blood tests are MESOMARK, the mesothelin test and fibulin-3 tests. MESOMARK is the only FDA-approved blood test for mesothelioma. It looks for proteins the mesothelium, or lining around your body’s cavities, makes. The mesothelin test, also known as the N-ERC/mesothelin test, also looks for this protein.
MESOMARK and the N-ERC/mesothelin test can usually indicate if mesothelioma is present. The fibulin-3 test can usually confirm when it’s not present. The fibulin-3 test is very specific. If fibulin-3 levels are low, there’s little chance of mesothelioma.
Blood Tests Commonly Used for Mesothelioma
All these blood tests use ELISA, a testing process that finds and measures certain proteins in the blood. A doctor or nurse takes a blood sample. That sample is mixed with antibodies that attach to the protein being tested. Machines then measure how much of the protein is there, helping doctors see what’s going on.

Connect with top-rated mesothelioma specialists at a cancer center near you, who will personalize treatment options based on your diagnosis.
Find Your CenterThe MESOMARK test is most helpful for monitoring epithelioid and biphasic subtypes of mesothelioma. These are the most common subtypes of this malignant cancer. Healthy cells produce low SMRP levels, but so do some sarcomatoid mesothelioma tumors. So SMRP levels may stay low even if mesothelioma is present.
According to Dr. Smart, “A MESOMARK blood test is performed by the physician or nurse practitioner drawing a sample of blood. That blood is sent to a lab where the levels of SMRP protein are measured.”
Developed in Japan, the N-ERC/mesothelin test is a blood test for mesothelioma that identifies mesothelin in the bloodstream. Mesothelin is a protein released in the body as tumor cells grow. The test is currently undergoing trials for implementation worldwide.
Although other cancers can also release mesothelin, the N-ERC/mesothelin test is more accurate than MESOMARK. It can help diagnose mesothelioma faster compared to other blood tests, especially when paired with imaging and a thorough history.
The Fibulin-3 blood test for mesothelioma evaluates the amount of fibulin-3 protein present. Research shows individuals diagnosed with pleural mesothelioma have increased average levels of fibulin-3.
Several researchers have found the sensitivity of the fibulin-3 test can vary. This variation potentially makes the test less effective for detecting mesothelioma. But when paired with other tests, it can play a role in confirming a mesothelioma diagnosis or ruling out a diagnosis.
The doctor came into my hospital room and said he had good news and bad news. He said, ‘You’ll walk again, but your blood work makes us think you have some sort of cancer.’
Researchers continue to study new blood tests for mesothelioma to improve early detection and diagnosis. These tests aren’t yet widely available, but they show promise in identifying subtle signs of cancer.
New Blood Tests for Mesothelioma
New studies suggest integrating multiple markers can improve accuracy and help tailor treatments. They’re also exploring additional signs or immunohistochemical markers of this disease. These advances and new, more effective combination tests will potentially enhance early detection and the outlook for people with this cancer or mesothelioma prognosis.
For example, a 2023 study published in Journal of Thoracic Oncology explored how microRNA patterns may help detect mesothelioma in earlier stages. MicroRNA are tiny pieces inside your cells that help control which proteins your body makes. Research like this may eventually lead to more accurate and less invasive tests.
Blood tests for mesothelioma can provide helpful indications, but they’re not as conclusive as a biopsy. A biopsy remains the gold standard for diagnosis.
Insurance may cover some blood tests, like MESOMARK, with a prescription from a health care professional. But coverage varies widely depending on your insurance provider and policy specifics.
Most mesothelioma blood tests are performed at specialized cancer centers, hospitals or laboratories that collaborate with mesothelioma experts. Patient Advocates or your doctor can help you find an appropriate facility for testing.
Stay up-to-date on treatment, research, clinical trials, doctors and survivors
The information on this website is proprietary and protected. It is not a substitute for professional medical advice, diagnosis or treatment. Any unauthorized or illegal use, copying or dissemination will be prosecuted. Please read our privacy policy and terms of service for more information about our website.
This website and its content may be deemed attorney advertising. Prior results do not predict a similar outcome.
The Mesothelioma Center’s claim as the most trusted resource is based on our more than 150 5-star Google and BBB reviews. Our organization also helps more than half of all mesothelioma patients annually diagnosed.
Your web browser is no longer supported by Microsoft. Update your browser for more security, speed and compatibility.
If you are looking for mesothelioma support, please contact our Patient Advocates at (855) 404-4592
The Mesothelioma Center at Asbestos.com has provided patients and their loved ones the most updated and reliable information on mesothelioma and asbestos exposure since 2006.
Our team of Patient Advocates includes a medical doctor, a registered nurse, health services administrators, veterans, VA-accredited Claims Agents, an oncology patient navigator and hospice care expert. Their combined expertise means we help any mesothelioma patient or loved one through every step of their cancer journey.
More than 30 contributors, including mesothelioma doctors, survivors, health care professionals and other experts, have peer-reviewed our website and written unique research-driven articles to ensure you get the highest-quality medical and health information.
My family has only the highest compliment for the assistance and support that we received from The Mesothelioma Center. This is a staff of compassionate and knowledgeable individuals who respect what your family is experiencing and who go the extra mile to make an unfortunate diagnosis less stressful. Information and assistance were provided by The Mesothelioma Center at no cost to our family.LashawnMesothelioma patient’s daughter


Asbestos.com. (2026, February 13). Mesothelioma Blood Tests and Biomarkers. Retrieved February 23, 2026, from https://www.asbestos.com/mesothelioma/blood-test/
"Mesothelioma Blood Tests and Biomarkers." Asbestos.com, 13 Feb 2026, https://www.asbestos.com/mesothelioma/blood-test/.
Asbestos.com. "Mesothelioma Blood Tests and Biomarkers." Last modified February 13, 2026. https://www.asbestos.com/mesothelioma/blood-test/.

Dr. Landau is the Medical Director of Virtual Hematology at the Medical University of South Carolina, where he leads programs that expand access to cancer care through telehealth. With more than 18 years of experience in oncology and hematology, he specializes in hematologic and genitourinary cancers, including bladder, prostate and kidney cancers. He has held multiple leadership roles in cancer program development and previously served as section chief of hematology and oncology at Orlando Health UF Health Cancer Center, where he founded its telehealth program.
Our fact-checking process begins with a thorough review of all sources to ensure they are high quality. Then we cross-check the facts with original medical or scientific reports published by those sources, or we validate the facts with reputable news organizations, medical and scientific experts and other health experts. Each page includes all sources for full transparency.
Please read our editorial guidelines to learn more about our content creation and review process.
