Barbara Lapalla’s chemotherapy side effects were debilitating. Her CT scan results showed it didn’t stop or slow her pleural mesothelioma from metastasizing too far for surgery. She attributes her miraculous turnaround to Keytruda (pembrolizumab). “Keytruda has worked like a charm for me, although I’m not exactly sure why,” Barbara said. “For me, it’s the magic bullet.”
Mesothelioma Metastasis
Medically Reviewed By: Dr. Robert B. Cameron | Written by: Dr. Daniel Landau | Last Update: 04/08/2025 | 8 Min Read
Metastatic mesothelioma occurs when malignant mesothelioma cells spread from the primary tumor in the lining of the lungs or abdomen to other parts of the body. When mesothelioma cells metastasize or spread, it's typically via lymph nodes, and cancer stage, cell type and treatment play a role.
Access information specific to your diagnosis.
Get Your Free Mesothelioma GuideMedically Reviewed By: Dr. Robert B. Cameron | Written by: Dr. Daniel Landau | Last Update: 04/08/2025 | 8 Min Read
Written by: Dr. Daniel Landau | Medically Reviewed By Dr. Robert B. Cameron | Edited By Walter Pacheco | Last Update: April 8, 2025

Exclusive Content | Dr. Farid Gharagozloo: Metastasis and Surgery Eligibility

Exclusive Content
Dr. Farid Gharagozloo: Metastasis and Surgery Eligibility
"The Patient Advocates are absolutely amazing and helpful! I ...." see more
Pamela K. - Mesothelioma Patient
"I found out about The Mesothelioma Center while researching ...." see more
Karen F. - Mesothelioma Patient
"I reached out and talked to Aaron a couple of weeks before m...." see more
Stan B. - Mesothelioma Patient
"My brother was recently diagnosed with mesothelioma. I began...." see more
Cindy W. - Sister of a Mesothelioma Patient
"My Dad was diagnosed with mesothelioma, and thankfully The M...." see more
Patrick K. - Son of a Mesothelioma Patient
Where Does Mesothelioma Metastasize?
Metastatic mesothelioma can spread to several organs, such as the liver, lungs, kidneys, adrenal glands or spleen. Metastasis happens when cancer cells travel from their point of origin to other sites in the body, moving through the bloodstream or lymph system.
It’s generally more common for mesothelioma to continue spreading throughout the cavity where it originally formed. Doctors call this local spread. After mesothelioma cells have spread, they can invade organs and form secondary tumors. This spread is the hallmark of the later stages of the disease.
Metastatic Pleural Mesothelioma
Doctors believed pleural mesothelioma was primarily a localized disease, but mounting research shows it frequently spreads to distant organs. A 2024 study found 13.3% of people with pleural mesothelioma had distant metastases (excluding the brain) at the time of diagnosis. This followed a 2012 study of 318 mesothelioma patients that found 55.4% had metastases to distant sites.
- Adrenal glands
- Bone
- Intestines
- Kidneys
- Liver
- Opposite lung
- Peritoneum (abdominal lining)
In a 2020 retrospective study of 164 pleural mesothelioma patients, about 67% had distant metastatic tumors. The most common sites were the opposite lung (35%), peritoneum (22%) bone (19%) and viscera (14%). An older study in 1991 reviewed 172 people who died of pleural mesothelioma and found the most common sites for mesothelioma metastasis include the liver (55.9%), adrenal glands (31.3%), kidneys (30.1%) and the opposite lung (26.8%).
Mesothelioma spreading to the brain and central nervous system is less common. Studies in 2022 and 2024 revealed metastasis to the brain occurs in only about 5% of pleural mesothelioma patients. Mesothelioma can also spread to other sites, such as the tongue and scalp.
Metastatic Peritoneal Mesothelioma
The most frequent sites of peritoneal metastases include the liver, abdominal lining and abdominal lymph nodes. Less common sites include the lungs, heart, brain, bone and kidneys.
- Abdominal lymph nodes
- Inner layer of the peritoneum (visceral peritoneum)
- Liver
In the early stages of the disease’s development, peritoneal mesothelioma doesn’t spread beyond the abdominal cavity. This area contains the stomach, spleen, liver, intestines and other abdominal organs.
As the disease progresses, cancer cells spread to near and distant organs. Distant metastases have been found in about 50% of peritoneal mesothelioma cases at autopsy.
Metastatic Pericardial and Testicular Mesothelioma
The local spread of pericardial mesothelioma usually involves the pleura, lung and the rest of the chest cavity. Pericardial mesothelioma metastasizes in about 25% to 45% of cases. Frequent sites are the regional lymph nodes, lungs and kidneys.
- Kidneys
- Liver
- Lungs
- Omentum (fatty tissues around the abdominal organs)
- Regional lymph nodes
- Vertebrae, chest (thorax) and lumbar
As testicular mesothelioma progresses, it tends to spread from the lining of the testes to the lymph nodes in the lower body. Metastasis in this mesothelioma type is rare. When it occurs, it can spread to the vertebrae of the spine, omentum, liver and lungs.
Find the top cancer centers trusted by mesothelioma patients nationwide.
Get Help NowWhen Does Mesothelioma Metastasize?
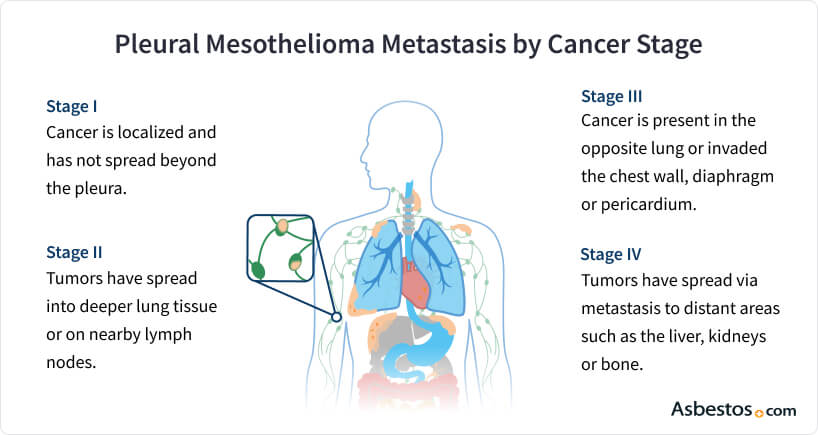
Mesothelioma is more likely to metastasize when the disease progresses. Mesothelioma stages measure this progression. In stages 1, 2 and 3, cancer cells spread locally within the body cavity where they developed and regionally to lymph nodes. In stage 4 mesothelioma, cancer cells can spread to distant lymph nodes and metastasize to distant organs.
Doctors detect cancer progression through diagnostic imaging tests. These include MRIs, PET and CT scans. Symptoms not generally associated with mesothelioma may be signs that cancer has spread. At that time, your doctor will perform tests or biopsies to look for distant metastases.
Continued Learning
Enhance your well-being and build strength with safe, effective exercises for mesothelioma patients.
Get Your Free GuideCauses of Mesothelioma Metastasis
Mesothelioma metastasis occurs when cancer cells enter the bloodstream through a process called angiogenesis. New capillaries form in the body from existing blood vessels, which typically benefits healthy growth and healing in the body. However this process can also help cancer cells grow.
“These microscopic cancer cells, once they’re in the bloodstream, they can go to other organs, whether it’s in the abdomen or the liver or the bone or the brain,” Dr. Jacques Fontaine, director of Moffitt Cancer Center’s Mesothelioma Research and Treatment Center, told The Mesothelioma Center. “Then [these cells] set up shop there, and they start growing and creating little cancers there. And that’s what a metastasis is.”
- Cancer Stage: The risk of metastasis is low in early-stage mesothelioma (stages 1 and 2) and high in advanced stages (stages 3 and 4).
- Tumor Cell Type: Epithelioid mesothelioma spreads more slowly than the more aggressive sarcomatoid or biphasic types.
- Response to Treatment: Chemotherapy, radiation, anti-angiogenesis drugs, Tumor Treating Fields and cytoreductive surgery can all reduce the risk of metastasis.
Factors such as cancer stage, tumor cell type and response to treatment influence the risk of metastasis. Patients have a lower risk if they have an early-stage diagnosis with a favorable cell type that responds well to treatment.
Continued Learning
What Are the Symptoms of Metastatic Mesothelioma?
Symptoms of metastatic mesothelioma include abdominal pain, changes in blood pressure and memory loss. However, it can be difficult for doctors to detect when mesothelioma has metastasized. Distant spread occurs late in cancer development and doesn’t always cause noticeable symptoms.
- Difficulty breathing
- Fatigue
- Fever
- Neurological symptoms (changes in vision, seizures, etc.)
- Pain
- Weakness
- Weight loss
“The doctor said, ‘Call an ambulance. Get her to the hospital right away,’” pleural mesothelioma survivor Carla Fasolo told The Mesothelioma Center. “They took me to the ER and told me they had found a large tumor on my chest’s right side and didn’t know if it had metastasized. [After] a CT scan and a biopsy, they determined it was mesothelioma.”
The symptoms of metastasis can vary based on where the cancer has spread. For example, metastases to the lungs can cause difficulty breathing and chest pain. Tumors in the brain may lead to neurological issues. Other symptoms are more generalized, affecting the entire body.
Some symptoms of mesothelioma metastases mimic common symptoms of mesothelioma and other cancers. Spread in the adrenal glands, for instance, can cause weight loss and muscle weakness that doctors may attribute to other conditions. Doctors often don’t discover metastases until after imaging scans or other tests.
Treating Metastatic Mesothelioma
A combination of therapies is often the most effective approach to treating mesothelioma. A mesothelioma specialist can recommend the best course of treatment after metastasis.
In combination with chemotherapy, Tumor Treating Fields can delay or prevent mesothelioma from spreading. Immunotherapy, a newer treatment against metastasis, may reduce the rate of metastasis when received before surgery.
- Chemotherapy: Destroys cancer cells throughout the body and delays metastasis
- Immunotherapy: Targets proteins crucial for cancer cell growth and spread
- Localized Chemotherapy: Treats tumors and metastases in the chest or abdomen
- Radiation: Shrinks tumors and prevents local spread of mesothelioma
- Tumor Treating Fields: Noninvasively reduces cancer spread, stimulates the body’s immune response and may increase the benefits of chemotherapy
Given the role angiogenesis plays in metastasis, researchers are studying anti-angiogenic medications. Drugs in clinical trials for mesothelioma metastasis include the anti-angiogenic semaxanib (SU5416) as well as an anti-copper agent, tetrathiomolybdate. In studies, these medications have stabilized the disease.
Once cancer has spread to distant parts of the body, treatment options tend to center around palliative care. These therapies relieve symptoms and provide comfort rather than cure the disease.
Common Questions About Mesothelioma Metastasis
- Can metastasis be prevented in mesothelioma patients?
-
Mesothelioma treatments can reduce, if not always prevent, local spread of disease and the risk of distant metastases. Options include chemotherapy, radiation, immunotherapy and Tumor Treating Fields.
- What is the prognosis for patients with metastatic mesothelioma?
-
Metastatic stage 4 mesothelioma has an average life expectancy of 14.9 months. However, an individual’s prognosis can vary based on mesothelioma location, cell type, age and overall health.
- Are there support groups or resources for patients with metastatic mesothelioma?
-
Yes, the Mesothelioma Center at Asbestos.com has support groups for people with mesothelioma and their loved ones. These include the Mesothelioma Support Group and the Mesothelioma Survivor, Caregiver & Family Support Facebook group.





