Get in Touch
Have questions? Call or chat with our Patient Advocates for answers.
Testicular mesothelioma is the rarest cancer caused by exposure to asbestos. It forms in the lining of the testes and is less common than pleural or peritoneal mesothelioma. Symptoms include a buildup of fluid and painful swelling of the testes. The 5-year survival rate for testicular mesothelioma is 49%.
Written by Karen Selby, RN | Medically Reviewed By Dr. Jacques Fontaine | Edited By Walter Pacheco | Last Update: June 27, 2024
Doctors do not yet understand how asbestos exposure can cause a primary tumor to develop on the tunica vaginalis. This area is the pouch of the serous membrane that covers the testes. Unlike pleural or peritoneal mesothelioma, this type does not simply correlate to asbestos exposure.
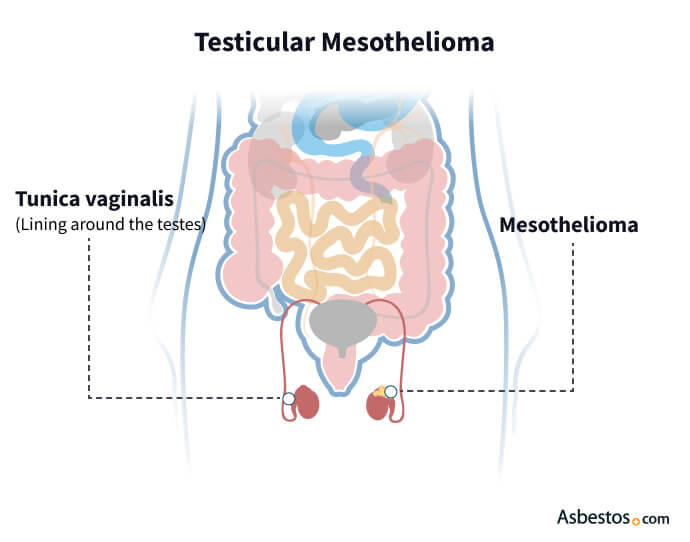
It appears as firm, white-yellow nodules on the surface of the tunica vaginalis. The nodules can eventually encase the contents of the scrotum and cause the membrane to thicken.
Local trauma and inflammation also may play a role in its development. Some cases present without any identifiable risk factors.

Get specialized treatment from experienced mesothelioma doctors.
Find a Doctor NowMen with this cancer have a significantly better prognosis than most people with other types of mesothelioma.
According to a 2019 study published in the journal Urology, nearly 49% of patients survive five years after diagnosis, and 33% survive 10 years. The average testicular mesothelioma life expectancy is between 20 months and two years.
Patients with the biphasic cell type had worse overall survival than other types.
Of the 113 testicular mesothelioma patients in the study, 75% of cases had the epithelioid cell type. Older patients and those with tumors greater than or equal to 4 centimeters in size were associated with a worse survival rate.
The most common testicular mesothelioma symptom is a hydrocele, a fluid buildup in the scrotum. There is no set of symptoms unique to testicular mesothelioma cancer.
Many people with this cancer initially receive the wrong diagnosis. Doctors often mistake it for a more common condition, such as a hernia.
More than half of the patients in the 2019 Urology study had a hydrocele, and about one-third had a painless scrotal mass.
1%
Percentage of respondents to The Mesothelioma Center’s 2023 patient survey who were diagnosed with testicular mesothelioma, the rarest form of the cancer.
This type is rare and doesn’t present unique symptoms. Doctors often diagnose testicular mesothelioma during or after surgery.
The definitive way of confirming a cancer diagnosis is to perform a biopsy. This procedure involves removing a tissue sample from the tumor and sending it to the lab for testing.
Evaluating the sample with immunohistochemical staining helps doctors determine if the patient has testicular mesothelioma or another disease.
The most common treatment for testicular mesothelioma is surgery. Nearly all (98.2%) of the 113 testicular mesothelioma patients in the 2019 study underwent surgical resection of the tumor.
This procedure removes the affected testicle and the entire spermatic chord. If cancer has spread to nearby lymph nodes, doctors will remove them with a lymphadenectomy surgery.
A 2021 research study noted that testicular mesothelioma requires extensive resection, including metastatic surgery if complete resection is possible. The study suggested a multimodality treatment plan for the malignancy, similar to a multimodal approach to pleural mesothelioma, offers the best patient outcomes.
Testicular mesothelioma patients I’ve spoken with are usually concerned about the rarity of this diagnosis. Some patients seem to have a longer life expectancy and better quality of life compared to patients with other types of mesothelioma.
Surgery may come before chemotherapy with cisplatin and pemetrexed, the longstanding standard-of-care treatment for mesothelioma. Doctors may offer radiation therapy next to kill any remaining cancer cells and prevent cancer from returning.
Only 5.3% of patients received radiation therapy in the 2019 study. Given such a small cohort, researchers could not determine if adjuvant therapy impacts overall survival.
In some cases, testicular mesothelioma is a secondary tumor, with the primary tumor located within the peritoneum (the membrane that lines the abdominal cavity). In these situations, doctors must treat the patient for peritoneal mesothelioma cancer.
Recommended ReadingThank you for your feedback. Would you like to speak with a Patient Advocate?
Your web browser is no longer supported by Microsoft. Update your browser for more security, speed and compatibility.
If you are looking for mesothelioma support, please contact our Patient Advocates at (855) 404-4592
The Mesothelioma Center at Asbestos.com has provided patients and their loved ones the most updated and reliable information on mesothelioma and asbestos exposure since 2006.
Our team of Patient Advocates includes a medical doctor, a registered nurse, health services administrators, veterans, VA-accredited Claims Agents, an oncology patient navigator and hospice care expert. Their combined expertise means we help any mesothelioma patient or loved one through every step of their cancer journey.
More than 30 contributors, including mesothelioma doctors, survivors, health care professionals and other experts, have peer-reviewed our website and written unique research-driven articles to ensure you get the highest-quality medical and health information.
My family has only the highest compliment for the assistance and support that we received from The Mesothelioma Center. This is a staff of compassionate and knowledgeable individuals who respect what your family is experiencing and who go the extra mile to make an unfortunate diagnosis less stressful. Information and assistance were provided by The Mesothelioma Center at no cost to our family.LashawnMesothelioma patient’s daughter


Selby, K. (2024, June 27). Testicular Mesothelioma. Asbestos.com. Retrieved July 26, 2024, from https://www.asbestos.com/mesothelioma/testicular/
Selby, Karen. "Testicular Mesothelioma." Asbestos.com, 27 Jun 2024, https://www.asbestos.com/mesothelioma/testicular/.
Selby, Karen. "Testicular Mesothelioma." Asbestos.com. Last modified June 27, 2024. https://www.asbestos.com/mesothelioma/testicular/.
The Mesothelioma Center at Asbestos.com has provided patients and their loved ones the most updated and reliable information on mesothelioma and asbestos exposure since 2006.
Our team of Patient Advocates includes a medical doctor, a registered nurse, health services administrators, veterans, VA-accredited Claims Agents, an oncology patient navigator and hospice care expert. Their combined expertise means we help any mesothelioma patient or loved one through every step of their cancer journey.
More than 30 contributors, including mesothelioma doctors, survivors, health care professionals and other experts, have peer-reviewed our website and written unique research-driven articles to ensure you get the highest-quality medical and health information.
My family has only the highest compliment for the assistance and support that we received from The Mesothelioma Center. This is a staff of compassionate and knowledgeable individuals who respect what your family is experiencing and who go the extra mile to make an unfortunate diagnosis less stressful. Information and assistance were provided by The Mesothelioma Center at no cost to our family.LashawnMesothelioma patient’s daughter


Selby, K. (2024, June 27). Testicular Mesothelioma. Asbestos.com. Retrieved July 26, 2024, from https://www.asbestos.com/mesothelioma/testicular/
Selby, Karen. "Testicular Mesothelioma." Asbestos.com, 27 Jun 2024, https://www.asbestos.com/mesothelioma/testicular/.
Selby, Karen. "Testicular Mesothelioma." Asbestos.com. Last modified June 27, 2024. https://www.asbestos.com/mesothelioma/testicular/.
The Mesothelioma Center at Asbestos.com has provided patients and their loved ones the most updated and reliable information on mesothelioma and asbestos exposure since 2006.
Our team of Patient Advocates includes a medical doctor, a registered nurse, health services administrators, veterans, VA-accredited Claims Agents, an oncology patient navigator and hospice care expert. Their combined expertise means we help any mesothelioma patient or loved one through every step of their cancer journey.
More than 30 contributors, including mesothelioma doctors, survivors, health care professionals and other experts, have peer-reviewed our website and written unique research-driven articles to ensure you get the highest-quality medical and health information.
My family has only the highest compliment for the assistance and support that we received from The Mesothelioma Center. This is a staff of compassionate and knowledgeable individuals who respect what your family is experiencing and who go the extra mile to make an unfortunate diagnosis less stressful. Information and assistance were provided by The Mesothelioma Center at no cost to our family.LashawnMesothelioma patient’s daughter


Selby, K. (2024, June 27). Testicular Mesothelioma. Asbestos.com. Retrieved July 26, 2024, from https://www.asbestos.com/mesothelioma/testicular/
Selby, Karen. "Testicular Mesothelioma." Asbestos.com, 27 Jun 2024, https://www.asbestos.com/mesothelioma/testicular/.
Selby, Karen. "Testicular Mesothelioma." Asbestos.com. Last modified June 27, 2024. https://www.asbestos.com/mesothelioma/testicular/.
The Mesothelioma Center at Asbestos.com has provided patients and their loved ones the most updated and reliable information on mesothelioma and asbestos exposure since 2006.
Our team of Patient Advocates includes a medical doctor, a registered nurse, health services administrators, veterans, VA-accredited Claims Agents, an oncology patient navigator and hospice care expert. Their combined expertise means we help any mesothelioma patient or loved one through every step of their cancer journey.
More than 30 contributors, including mesothelioma doctors, survivors, health care professionals and other experts, have peer-reviewed our website and written unique research-driven articles to ensure you get the highest-quality medical and health information.
My family has only the highest compliment for the assistance and support that we received from The Mesothelioma Center. This is a staff of compassionate and knowledgeable individuals who respect what your family is experiencing and who go the extra mile to make an unfortunate diagnosis less stressful. Information and assistance were provided by The Mesothelioma Center at no cost to our family.LashawnMesothelioma patient’s daughter


Selby, K. (2024, June 27). Testicular Mesothelioma. Asbestos.com. Retrieved July 26, 2024, from https://www.asbestos.com/mesothelioma/testicular/
Selby, Karen. "Testicular Mesothelioma." Asbestos.com, 27 Jun 2024, https://www.asbestos.com/mesothelioma/testicular/.
Selby, Karen. "Testicular Mesothelioma." Asbestos.com. Last modified June 27, 2024. https://www.asbestos.com/mesothelioma/testicular/.
The Mesothelioma Center at Asbestos.com has provided patients and their loved ones the most updated and reliable information on mesothelioma and asbestos exposure since 2006.
Our team of Patient Advocates includes a medical doctor, a registered nurse, health services administrators, veterans, VA-accredited Claims Agents, an oncology patient navigator and hospice care expert. Their combined expertise means we help any mesothelioma patient or loved one through every step of their cancer journey.
More than 30 contributors, including mesothelioma doctors, survivors, health care professionals and other experts, have peer-reviewed our website and written unique research-driven articles to ensure you get the highest-quality medical and health information.
My family has only the highest compliment for the assistance and support that we received from The Mesothelioma Center. This is a staff of compassionate and knowledgeable individuals who respect what your family is experiencing and who go the extra mile to make an unfortunate diagnosis less stressful. Information and assistance were provided by The Mesothelioma Center at no cost to our family.LashawnMesothelioma patient’s daughter


Selby, K. (2024, June 27). Testicular Mesothelioma. Asbestos.com. Retrieved July 26, 2024, from https://www.asbestos.com/mesothelioma/testicular/
Selby, Karen. "Testicular Mesothelioma." Asbestos.com, 27 Jun 2024, https://www.asbestos.com/mesothelioma/testicular/.
Selby, Karen. "Testicular Mesothelioma." Asbestos.com. Last modified June 27, 2024. https://www.asbestos.com/mesothelioma/testicular/.
The Mesothelioma Center at Asbestos.com has provided patients and their loved ones the most updated and reliable information on mesothelioma and asbestos exposure since 2006.
Our team of Patient Advocates includes a medical doctor, a registered nurse, health services administrators, veterans, VA-accredited Claims Agents, an oncology patient navigator and hospice care expert. Their combined expertise means we help any mesothelioma patient or loved one through every step of their cancer journey.
More than 30 contributors, including mesothelioma doctors, survivors, health care professionals and other experts, have peer-reviewed our website and written unique research-driven articles to ensure you get the highest-quality medical and health information.
My family has only the highest compliment for the assistance and support that we received from The Mesothelioma Center. This is a staff of compassionate and knowledgeable individuals who respect what your family is experiencing and who go the extra mile to make an unfortunate diagnosis less stressful. Information and assistance were provided by The Mesothelioma Center at no cost to our family.LashawnMesothelioma patient’s daughter


Selby, K. (2024, June 27). Testicular Mesothelioma. Asbestos.com. Retrieved July 26, 2024, from https://www.asbestos.com/mesothelioma/testicular/
Selby, Karen. "Testicular Mesothelioma." Asbestos.com, 27 Jun 2024, https://www.asbestos.com/mesothelioma/testicular/.
Selby, Karen. "Testicular Mesothelioma." Asbestos.com. Last modified June 27, 2024. https://www.asbestos.com/mesothelioma/testicular/.
The Mesothelioma Center at Asbestos.com has provided patients and their loved ones the most updated and reliable information on mesothelioma and asbestos exposure since 2006.
Our team of Patient Advocates includes a medical doctor, a registered nurse, health services administrators, veterans, VA-accredited Claims Agents, an oncology patient navigator and hospice care expert. Their combined expertise means we help any mesothelioma patient or loved one through every step of their cancer journey.
More than 30 contributors, including mesothelioma doctors, survivors, health care professionals and other experts, have peer-reviewed our website and written unique research-driven articles to ensure you get the highest-quality medical and health information.
My family has only the highest compliment for the assistance and support that we received from The Mesothelioma Center. This is a staff of compassionate and knowledgeable individuals who respect what your family is experiencing and who go the extra mile to make an unfortunate diagnosis less stressful. Information and assistance were provided by The Mesothelioma Center at no cost to our family.LashawnMesothelioma patient’s daughter


Selby, K. (2024, June 27). Testicular Mesothelioma. Asbestos.com. Retrieved July 26, 2024, from https://www.asbestos.com/mesothelioma/testicular/
Selby, Karen. "Testicular Mesothelioma." Asbestos.com, 27 Jun 2024, https://www.asbestos.com/mesothelioma/testicular/.
Selby, Karen. "Testicular Mesothelioma." Asbestos.com. Last modified June 27, 2024. https://www.asbestos.com/mesothelioma/testicular/.
The Mesothelioma Center at Asbestos.com has provided patients and their loved ones the most updated and reliable information on mesothelioma and asbestos exposure since 2006.
Our team of Patient Advocates includes a medical doctor, a registered nurse, health services administrators, veterans, VA-accredited Claims Agents, an oncology patient navigator and hospice care expert. Their combined expertise means we help any mesothelioma patient or loved one through every step of their cancer journey.
More than 30 contributors, including mesothelioma doctors, survivors, health care professionals and other experts, have peer-reviewed our website and written unique research-driven articles to ensure you get the highest-quality medical and health information.
My family has only the highest compliment for the assistance and support that we received from The Mesothelioma Center. This is a staff of compassionate and knowledgeable individuals who respect what your family is experiencing and who go the extra mile to make an unfortunate diagnosis less stressful. Information and assistance were provided by The Mesothelioma Center at no cost to our family.LashawnMesothelioma patient’s daughter


Selby, K. (2024, June 27). Testicular Mesothelioma. Asbestos.com. Retrieved July 26, 2024, from https://www.asbestos.com/mesothelioma/testicular/
Selby, Karen. "Testicular Mesothelioma." Asbestos.com, 27 Jun 2024, https://www.asbestos.com/mesothelioma/testicular/.
Selby, Karen. "Testicular Mesothelioma." Asbestos.com. Last modified June 27, 2024. https://www.asbestos.com/mesothelioma/testicular/.
The Mesothelioma Center at Asbestos.com has provided patients and their loved ones the most updated and reliable information on mesothelioma and asbestos exposure since 2006.
Our team of Patient Advocates includes a medical doctor, a registered nurse, health services administrators, veterans, VA-accredited Claims Agents, an oncology patient navigator and hospice care expert. Their combined expertise means we help any mesothelioma patient or loved one through every step of their cancer journey.
More than 30 contributors, including mesothelioma doctors, survivors, health care professionals and other experts, have peer-reviewed our website and written unique research-driven articles to ensure you get the highest-quality medical and health information.
My family has only the highest compliment for the assistance and support that we received from The Mesothelioma Center. This is a staff of compassionate and knowledgeable individuals who respect what your family is experiencing and who go the extra mile to make an unfortunate diagnosis less stressful. Information and assistance were provided by The Mesothelioma Center at no cost to our family.LashawnMesothelioma patient’s daughter


Selby, K. (2024, June 27). Testicular Mesothelioma. Asbestos.com. Retrieved July 26, 2024, from https://www.asbestos.com/mesothelioma/testicular/
Selby, Karen. "Testicular Mesothelioma." Asbestos.com, 27 Jun 2024, https://www.asbestos.com/mesothelioma/testicular/.
Selby, Karen. "Testicular Mesothelioma." Asbestos.com. Last modified June 27, 2024. https://www.asbestos.com/mesothelioma/testicular/.
The Mesothelioma Center at Asbestos.com has provided patients and their loved ones the most updated and reliable information on mesothelioma and asbestos exposure since 2006.
Our team of Patient Advocates includes a medical doctor, a registered nurse, health services administrators, veterans, VA-accredited Claims Agents, an oncology patient navigator and hospice care expert. Their combined expertise means we help any mesothelioma patient or loved one through every step of their cancer journey.
More than 30 contributors, including mesothelioma doctors, survivors, health care professionals and other experts, have peer-reviewed our website and written unique research-driven articles to ensure you get the highest-quality medical and health information.
My family has only the highest compliment for the assistance and support that we received from The Mesothelioma Center. This is a staff of compassionate and knowledgeable individuals who respect what your family is experiencing and who go the extra mile to make an unfortunate diagnosis less stressful. Information and assistance were provided by The Mesothelioma Center at no cost to our family.LashawnMesothelioma patient’s daughter


Selby, K. (2024, June 27). Testicular Mesothelioma. Asbestos.com. Retrieved July 26, 2024, from https://www.asbestos.com/mesothelioma/testicular/
Selby, Karen. "Testicular Mesothelioma." Asbestos.com, 27 Jun 2024, https://www.asbestos.com/mesothelioma/testicular/.
Selby, Karen. "Testicular Mesothelioma." Asbestos.com. Last modified June 27, 2024. https://www.asbestos.com/mesothelioma/testicular/.
A medical doctor who specializes in mesothelioma or cancer treatment reviewed the content on this page to ensure it meets current medical standards and accuracy.
Please read our editorial guidelines to learn more about our content creation and review process.
Dr. Jacques Fontaine is a thoracic surgeon at Moffitt Cancer Center in Tampa, Florida, where he heads up the Mesothelioma Research and Treatment Center. He specializes in minimally invasive robotic surgery and aggressive surgeries for mesothelioma.
A medical doctor who specializes in mesothelioma or cancer treatment reviewed the content on this page to ensure it meets current medical standards and accuracy.
Please read our editorial guidelines to learn more about our content creation and review process.
Dr. Jacques Fontaine is a thoracic surgeon at Moffitt Cancer Center in Tampa, Florida, where he heads up the Mesothelioma Research and Treatment Center. He specializes in minimally invasive robotic surgery and aggressive surgeries for mesothelioma.
Mesothelioma Center - Vital Services for Cancer Patients & Families doesn’t believe in selling customer information. However, as required by the new California Consumer Privacy Act (CCPA), you may record your preference to view or remove your personal information by completing the form below.
