Mesothelioma Stages
Mesothelioma staging is the process of determining how far your cancer has spread. The 4-stage TNM system classifies mesothelioma from localized tumors at stage 1 to widespread at stage 4. Staging helps your doctor recommend the best treatment plan to help you achieve the best outcome.
What Are the Stages of Mesothelioma?
Mesothelioma has four stages. The stages range from 1 to 4. Stage 1 is the earliest or least advanced mesothelioma stage, and stage 4 is the most severe and means tumors have spread far in the body.
The 4 Stages of Mesothelioma
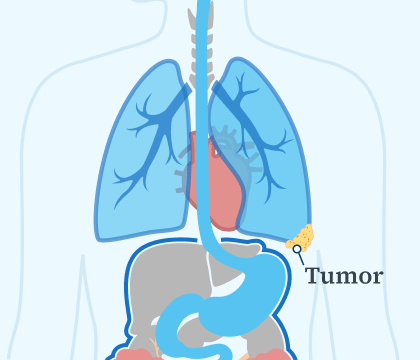
- Stage 1: Tumors are localized and haven’t spread.
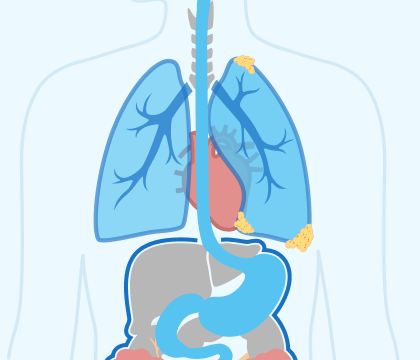
- Stage 2: Tumors can be seen in nearby tissues and possibly lymph nodes.
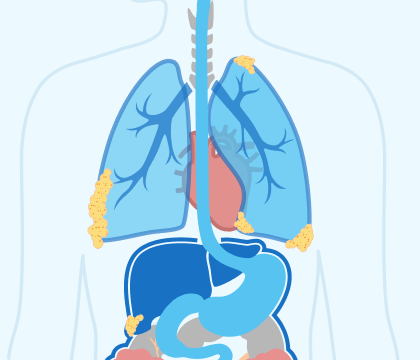
- Stage 3: More extensive cancer spread. Tumors can be seen within the chest and other tissues.
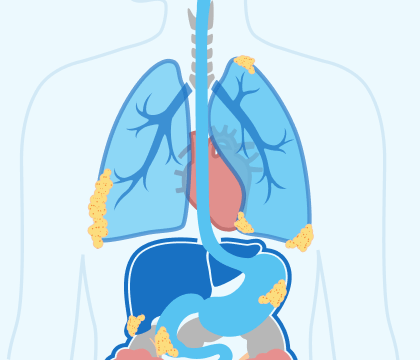
- Stage 4: Tumors have spread to distant organs.
Access top mesothelioma doctors, and get help scheduling appointments.
Find a Top DoctorYour mesothelioma stage describes where signs of the cancer can be seen in your body or how far it’s spread. Doctors use a system for pleural mesothelioma commonly called the TNM system, which stands for Tumor, Node and Metastasis. This system, commonly used for other cancers as well, classifies mesothelioma into 4 stages.
As mesothelioma progresses or moves from earlier stages to later stages, it can affect what treatment options are most likely to offer someone the best outcome. Typically, surgery and other aggressive therapies may be possible in early stages (stages 1 and 2). Having more therapy options can positively affect your predicted likely outcome or prognosis.
For advanced stages (stages 3 and 4), treatment often focuses more on slowing the disease and managing mesothelioma symptoms. This can help enhance quality of life. You may want to seek a second opinion to confirm your stage and explore all of your available treatment options.
How Is My Mesothelioma Stage Determined?
Your doctor will use several tests, including physical examinations, blood work, imaging scans and biopsies, to determine the stage of your mesothelioma. A thoracoscopy, a minimally invasive procedure that allows doctors to look inside your chest cavity may also be done and can help staging.
The TNM system is the most widely used for pleural mesothelioma. Each letter in the system’s name describes what doctors are looking at to determine tumor size are and where they’ve spread throughout the body. This helps determine which stage your mesothelioma is in.
What the TNM Staging System Measures
- Tumor: Measures the size and location of the primary tumor.
- Node: Determines whether cancer has spread to lymph nodes.
- Metastasis: Identifies if cancer has traveled to distant organs.
Pleural mesothelioma is the most common type of mesothelioma. Most people with mesothelioma will have their cancer staged using the TNM system. Other mesothelioma types are staged using different ways of describing how cancer has spread.
For peritoneal mesothelioma, for example, doctors use the Peritoneal Cancer Index. This helps doctors assess tumor spread in the abdomen. This system assigns scores based on the size and location of tumors throughout the abdominal cavity.

Get a free guide with the latest mesothelioma treatments and clinical trials.
Get Yours NowWhat Are the Stages of Pleural Mesothelioma?
The stages of pleural mesothelioma range from stage 1 to stage 4. The 4 stages of pleural mesothelioma describe how far the cancer has spread to other parts of the body. Stage 1 is the least advanced staged, and stage 4 is the most advanced. “The way we determine the stage is with a CT or PET scan,” thoracic surgeon Dr. Jacques Fontaine, director of the Mesothelioma Research and Treatment Center at the Moffitt Cancer Center, shared with us.
Mesothelioma stages directly impact prognosis. According to the Canadian Cancer Society, the average life expectancy ranges from 21 to 51 months after a stage 1 diagnosis to 8 to 12 months when diagnosed with stage 4 mesothelioma.
Stage 1 Mesothelioma
Stage 1 pleural mesothelioma is the earliest stage. The cancer is localized or still at the site where it first developed. Most likely, it is located on the lining of the chest cavity or pleura. It hasn’t spread to lymph nodes or distant organs.
Symptoms are usually mild or nonexistent, which makes early detection difficult. A mesothelioma diagnosis at this stage often has the best prognosis.
Characteristics of Stage 1 Pleural Mesothelioma
- Average survival rate: 21 months
- Cancer is localized to the pleura
- Symptoms are mild or nonexistent
- Treatment options: Surgery, chemotherapy and radiation
Pleural mesothelioma survivor Daniel McCarthy was diagnosed at an earlier stage, making surgery an option for him. “My wife is a nurse and noticed I was short of breath,” Daniel said. “She convinced me to see a doctor, and it basically saved my life.”
With early detection, aggressive treatments such as surgery and multimodal therapy offer the best chance of long-term survival. Seeking care from a mesothelioma specialist can help ensure you explore all available options.
Stage 2 Mesothelioma
At stage 2, pleural mesothelioma has started to spread beyond the pleura into nearby lung or diaphragm tissue. Symptoms such as mild chest pain, coughing and shortness of breath may begin to appear. Early-stage treatment remains aggressive, and multiple options are available.
Multimodal therapy, which combines surgery, chemotherapy and radiation, is often recommended. Patients in stage 2 still have curative treatment options, and clinical trials may offer additional opportunities.
Characteristics of Stage 2 Pleural Mesothelioma
- Average survival rate: 19 months
- Cancer has spread into nearby lung or diaphragm tissue
- Symptoms may include mild chest pain and coughing
- Treatment options: Surgery, chemotherapy and radiation
Diagnosed with stage 2 pleural mesothelioma in 2020, survivor Cheryl Pilkington tells us she and her sister often played in plaster dust in her father’s foundry shop. They were unaware this dust also contained asbestos.
“They never suspected [pleural mesothelioma],” Cheryl shares. “A female who was not in any business where there was asbestos exposure. They were shocked when the biopsy came back, but only until they heard my history.”
Stage 3 Mesothelioma
Stage 3 pleural mesothelioma means the cancer has spread further into nearby structures such as the chest wall, esophagus or deeper into the diaphragm. Symptoms become more noticeable, including persistent chest pain, difficulty breathing and fatigue.
“If a doctor refers to peritoneal mesothelioma as stage 3, it usually means tumors have spread throughout the abdominal lining and to nearby lymph nodes,” oncologist Dr. Daniel Landau, medical director of Virtual Hematology at the Medical University of South Carolina, tells us.
Characteristics of Stage 3 Pleural Mesothelioma
- Average survival rate: 16 months
- Cancer has spread to nearby organs and lymph nodes
- Symptoms include chest pain, fatigue and breathing difficulties
- Treatment options: Chemotherapy, immunotherapy and palliative care
Surgery is often not an option at this stage, but chemotherapy, immunotherapy and palliative treatments can help manage symptoms and slow disease progression. Some patients may qualify for clinical trials testing new therapies.
“When I was first diagnosed with stage 3 inoperable cancer, I was told I had a year to live,” said pleural mesothelioma survivor Russell Lamkins. “I figured I’d better hurry up and finish the projects I was working on. But now, my goal is to make it to the 10-year mark.”
Stage 4 Mesothelioma
Stage 4 is the most advanced stage of pleural mesothelioma. Cancer has spread to distant organs such as the liver, brain or bones. Symptoms are severe and may include significant weight loss, extreme fatigue and breathing difficulties.
Characteristics of Stage 4 Pleural Mesothelioma
- Average survival rate: ~12 months
- Cancer has spread to distant organs
- Symptoms include severe fatigue, weight loss and respiratory issues
- Treatment options: Palliative care, immunotherapy and clinical trials
At this stage, treatment often focuses on improving the quality of life through palliative care, pain management and oxygen therapy. Some patients explore immunotherapy or clinical trials, which may provide additional options for extending survival.
Pleural mesothelioma survivor Andy A. shares with us that immunotherapy has improved his health following his diagnosis in 2010. He tells us, “I guess I’m an anomaly. I’m doing great right now. I really am. I don’t look like a Stage 4 cancer patient. I consider myself extremely lucky for a lot of reasons.”
What Is the Staging System for Pleural Mesothelioma?
The TNM staging system is used to stage pleural mesothelioma. Pleural mesothelioma is the only type with an official staging system. The American Joint Committee on Cancer uses the TNM system to classify mesothelioma based on tumor size, lymph node involvement and spread or metastasis.
The 9th edition of the TNM system, released in January 2025, includes updates that improve staging accuracy. These changes provide specialists with better tools to understand how mesothelioma develops and which treatments may be most effective.
Dr. Jeffrey Velotta, a pleural mesothelioma expert and thoracic surgeon at Kaiser Permanente Oakland Medical Center, says, “The new TNM staging system for pleural mesothelioma standardizes tumor measurements which can help improve treatment guidelines and prognostic information.”
Do All Types of Mesothelioma Have Staging Systems?
While pleural mesothelioma has a formal staging system, other types of mesothelioma don’t. Pericardial and testicular mesothelioma are difficult to stage. Doctors will often make individualized assessments for their patients based on whether their cancer is localized or advanced.
Doctors often use the peritoneal cancer index to stage peritoneal mesothelioma. PCI scores range from 1 to 39, which directly correlate to prognosis. Patients with PCI scores higher than 30 had the lowest survival rates at 1, 2 and 5 years, while those with scores lower than 20 had the highest survival rates.
Staging Pericardial, Peritoneal and Testicular Mesothelioma
- Pericardial Mesothelioma: Doctors often rely on modified standard cancer indexes to describe tumor size and spread.
- Peritoneal Mesothelioma: Frequently staged using the peritoneal cancer index.
- Testicular Mesothelioma: Sometimes staged using a modified TNM system.
Some doctors use the Peritoneal Surface Oncology Group International’s modified TNM system to categorize other types into 3 stages. This system aims to determine which patients are most likely to benefit from surgery.
Testicular mesothelioma is also sometimes staged using a modified TNM system. This system includes an added value, “S,” for serum tumor marker levels.

Connect with trusted specialists who truly care about your health. Get fast, stress-free appointment help.
Find a Doctor NowHow Does My Mesothelioma Stage Affect My Treatment Options & Prognosis?
Patients with early-stage mesothelioma typically have more treatment options available, which can improve outcomes or prognosis. Aggressive treatments such as surgery can prolong survival.
Dr. Fontaine, director of the Mesothelioma Research and Treatment Center at Moffitt Cancer Center, spoke with us about the importance of personalized care. He explained, “The mesothelioma patients I treat who are good candidates for surgery are usually in the early stages, when the cancer is confined to the lung lining, hasn’t reached the lymph nodes, and hasn’t spread to other organs.”
The Role of Staging in Treatment Plans
- Stages 1-2: Surgery, chemo and radiation therapy are often options.
- Stage 3: Treatment focuses on slowing tumor growth with chemo and immunotherapy.
- Stage 4: Care is centered on improving quality of life through symptom and pain management, as well as oxygen therapy.
According to the American Cancer Society, 5-year survival rates for pleural mesothelioma range from 7% to 24, depending on the disease stage at diagnosis. The typical mesothelioma life expectancy ranges from 22.2 months at stage 1 to 14.9 months at stage 4.
Patients should note that mesothelioma survival rate data is based on cases diagnosed years ago and can’t predict individual survival. Recent advancements in treatment have also helped people at all stages live longer with mesothelioma. Clinical trials for people at every stage of mesothelioma are also showing promise in improving outcomes.
- Staging mesothelioma requires CT scans PET scans, according to a review published in the Journal of Clinical Medicine.
- Assessing the correct stage informs doctors about a mesothelioma patient’s prognosis and life expectancy.
“This is crucial because you need to know the extent of the disease in your body in order to get the most ideal tailored treatment regimen; thus, all patients should have, at a minimum, a CT scan and PET scan to start with.”
Common Questions About Mesothelioma Stages
- At what stage is mesothelioma diagnosed?
-
Mesothelioma can be diagnosed at any stage, from I through IV.
Answered By: Anna Nowak, internationally renowned asbestos researcher and mesothelioma advocate
- How fast does mesothelioma progress?
-
Every individual’s mesothelioma progresses at a different rate. Some have very slow-growing diseases, and others grow more rapidly. Sarcomatoid mesothelioma usually progresses more quickly than epithelioid mesothelioma.
Answered By: Anna Nowak, internationally renowned asbestos researcher and mesothelioma advocate
- Is stage 4 mesothelioma always terminal?
-
Mesothelioma is considered a terminal cancer because it has no cure. Treatment success varies between patients, but remission is possible. Palliative treatment options are also available and may improve symptoms and quality of life.
- How is the stage of mesothelioma different from the type of mesothelioma?
-
The stage describes how far the cancer has spread, while the type refers to where it develops (pleural, peritoneal, pericardial or testicular).
- How do I explain my stage of mesothelioma to my family?
-
Use simple terms, focusing on the treatment stage and the next steps. Support groups can help navigate these conversations.
- Should I get a second opinion about my stage or diagnosis?
-
Yes. Second opinions from mesothelioma specialists can confirm your stage and expand treatment options.