Managing Mesothelioma Pain With Palliative Treatment
Palliative care for mesothelioma includes surgery, radiation, chemo and immunotherapy. The goal is to improve quality of life. Starting palliative care early can ease symptoms. While it can be paired with curative treatment, palliative care’s goal isn't to cure mesothelioma.
What Is Palliative Treatment for Mesothelioma?
Palliative care is a type of mesothelioma treatment that focuses on your physical comfort, not necessarily the cancer. A diverse team of specialists work together to ease your symptoms and treatment side effects using a variety of different strategies.
Palliative Care Strategies for Mesothelioma
- Nutritional support: Working with a licensed dietitian who specializes in mesothelioma nutrition can help you maintain your strength and overall health.
- Pain management: This includes medications, nerve blocks or complementary therapies.
- Physical therapy: Exercise and physical therapy can help improve mobility and strength.
- Respiratory support: This includes breathing exercises and supplemental oxygen.
- Tumor management: Reducing tumor size and spread can have curative as well as palliative benefits. Traditional therapies like chemo and surgery to shrink or remove tumors can ease symptoms.
People report feeling more comfortable thanks to palliative care for malignant mesothelioma while they go through tough treatments like recovering from aggressive surgery. Your doctors can help you choose the treatments that will help you the most.
How Can Palliative Treatment Benefit Mesothelioma Patients?
Palliative treatment not only eases mesothelioma symptoms, but it can improve survival. An Australian study found that when people got help for poor appetite, their survival rates improved. The authors of a 2024 study in Current Oncology concluded palliative care should be included in every mesothelioma treatment plan.
A 2023 study in the British Journal of Community Nursing showed palliative care helps early-stage mesothelioma patients. For many, palliative care for mesothelioma also helps them spend more time at home instead of in the hospital.
Many people with mesothelioma undergo multimodal therapy, or a combination of therapies. They may experience side effects from each therapy or intensified overlapping side effects. Palliative care can help manage these effects.
The palliative treatment that will benefit you the most depends on the specific type of mesothelioma you have, the treatments you’re undergoing, and how far your cancer has progressed. Talk to your mesothelioma care team about how you’re feeling and your personal goals.
Who Provides Palliative Care for Mesothelioma Patients?
Providing palliative care for mesothelioma is a group effort typically involving a team of experts. This team often includes cancer doctors, surgeons, nurses, pain management specialists and licensed dietitians. They work as a unit to ensure you get the care you need.
Physical therapists, physical rehabilitation specialists and respiratory therapists also play critical roles in palliative care. Exercise during treatment, for example, not only helps people improve their strength and overall health, but it can reduce mesothelioma symptoms. Breathing exercises with a respiratory therapist can improve lung function. Talk to your care team about possibly working with other types of palliative care specialists.

Receive expert care from doctors who truly understand mesothelioma.
Find a Specialist NowTreatments for Mesothelioma That Are Curative and Palliative
Palliative treatment can include many of the same treatments for mesothelioma used to try to cure or slow the disease. Surgery, chemo, immunotherapy, and radiation can all reduce symptoms and improve quality of life. Surgeries like thoracentesis or pleurodesis remove or prevent fluid buildup, easing breathing.
Low-dose chemo and radiation can shrink tumors, which may relieve pressure or reduce pain. Immunotherapy may also support comfort and function with fewer side effects than chemo. These treatments, while often considered curative, can play a vital role in mesothelioma palliative care, focusing on comfort, function and overall quality of life.
Chemotherapy
Chemotherapy is an anti-cancer treatment for mesothelioma, but it can also play a role in palliative care. The side effects of chemotherapy can be harsh. Medications can reduce the negative effects, so patients can benefit from chemo.
Chemotherapy Administration
- HIPEC: Hyperthermic intraperitoneal chemotherapy uses heated chemotherapy drugs infused into the abdomen after cytoreductive surgery.
- HITHOC: Hyperthermic intrathoracic chemotherapy is similar to HIPEC and involves heated saline solution in the chest cavity.
- Systemic Chemotherapy: Usually administered via intravenous infusion for pleural and pericardial mesothelioma.
Chemotherapy is most often used on its own but is also used following surgery. HIPEC can extend life expectancy for mesothelioma patients. HITHOC hasn’t been found to provide as much benefit but can be beneficial for some patients.
Immunotherapy
Immunotherapy can improve mesothelioma survival and quality of life. Many patients experience fewer side effects compared to chemo.
Some palliative treatments can affect immunotherapy. Opioids prescribed for pain and corticosteroids for inflammation have immunosuppressive effects. The impact of antibiotics on healthy gut bacteria may impact immunotherapy.
Radiation Therapy
Radiation can shrink tumors, helping to relieve the pain they can cause. While it can cause skin irritation and fatigue, it’s useful for improving quality of life.
Radiation is used almost exclusively in pleural mesothelioma. It does not work for pericardial cases and is hard to use in peritoneal mesothelioma.
Surgery
Palliative surgery for mesothelioma can relieve the symptoms caused by fluid build-up like pleural effusions. Fluid accumulation can cause difficulty breathing, pain and other complications.
Fluid-Draining Procedures
- Paracentesis: This minor surgery drains fluid from the abdominal lining.
- Pericardiocentesis: This procedure removes fluid buildup in the sac encasing the heart.
- Pleurodesis: Seals the pleural space to prevent fluid from building up there.
- Thoracentesis: A minimally invasive procedure to remove fluid from the lung lining
Cytoreductive surgery is an invasive surgery to remove as much of the tumor as possible. It can have a palliative effect by controlling symptoms.
Mesothelioma Pain Management Techniques
Surgery and medication can help relieve certain types of mesothelioma pain. Mild pain may be treated with over-the-counter pain relievers such as acetaminophen. More severe pain is usually treated with opioid drugs. Examples include morphine, oxycodone or tramadol. IV pain medication may be needed for severe pain.
Other pain management techniques can be helpful as well. While pain originates in the body, it’s interpreted in the brain. Cognitive and behavioral techniques may help you manage your pain.
Techniques to Manage Mesothelioma Pain
- Acupuncture
- Cognitive Behavioral Techniques
- Distraction or Refocusing
- Exercise and Physical Therapy
- Hypnosis
- Massage
- Meditation
- Reiki
- Respiratory Therapy
- Soaking in a Warm Bath
- Visualization Exercises
- Walking
- Warm Washcloths or Heating Pads
- Yoga
Palliative care may improve your symptoms and even increase mesothelioma life expectancy. Complementary and alternative medicine isn’t recommended to replace traditional treatment. But it may offer symptomatic relief and improve your quality of life.
Many patients find relief with a holistic approach to palliative care. Some combine medication for anxiety and depression along with talk therapy and yoga.
Enhance your well-being and build strength with safe, effective exercises for mesothelioma patients.
Get Your Free GuidePalliative Treatment and Nutrition
You can improve your mesothelioma diet with help from a licensed dietitian. Proper nutrition gives your body strength to heal and helps your immune system stay strong during treatment. A balanced diet is important because it gives your body the fuel it needs to fight illness and recover.
Mesothelioma treatments like chemo or radiation can affect how food tastes and how your body digests it. Some treatments may cause nausea, vomiting or a loss of appetite. These side effects can make it hard to eat enough healthy food.
To eat well, try to eat small meals more often, drink plenty of water and include foods with protein and calories. Prescription drugs can help increase appetite and ease nausea. Always talk with a licensed dietitian or your care team before making changes to your diet.
If you have mesothelioma, eating more produce can help to build a healthy body. Research shows that fruits and vegetables can help fight cancer.
How Is Palliative Care Different From Hospice or Supportive Care?
These types of mesothelioma care overlap but are distinct. Supportive care is an umbrella of care that includes palliative therapies for physical symptoms and side effects and adds emotional and psychological support to help people cope with a mesothelioma diagnosis. Supportive care takes a holistic approach to addressing your needs.
Hospice can also include types of palliative care and supportive care to make people more comfortable. But while palliative care can happen at any time on your mesothelioma journey, hospice care is end-of-life care.
Palliative Care vs. Hospice Care
Both hospice and palliative care for mesothelioma help people feel more comfortable, but they aren’t the same. Palliative care can help at any stage of mesothelioma. This care can begin soon after your diagnosis and continue throughout your treatment to help you feel better.
Hospice care solely focuses on providing comfort when people have stopped curative treatment. People in hospice are nearing the end of their lives, and their care focuses on providing the best quality of life possible.
Patient Advocate Karen Selby of The Mesothelioma Center says, “There’s still a lot of confusion about what palliative treatment is versus hospice care. I find it important to explain how patients typically do better integrating palliative care early on rather than waiting.”
Surgery, radiation, chemotherapy, and medication can all be part of palliative treatment. Therapies can improve breathing and reduce excess fluid in the chest and abdomen.
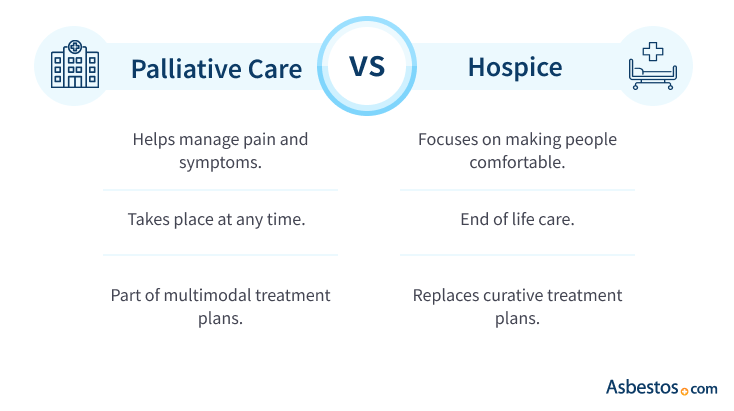
Palliative Care vs. Supportive Care
Palliative care eases mesothelioma symptoms and side effects of treatment. Supportive care helps you with the physical aspects of care and the psychological and emotional aspects of being a mesothelioma survivor. Mental health experts, Patient Advocates and support groups can help those dealing with stress, depression or anxiety.
Mental health support is a key part of supportive care. Living with mesothelioma can cause stress, fear, sadness and anxiety. These feelings can affect how you sleep, eat and handle treatment. Mesothelioma survivor Michael Cole tells us mental health support helped following his extrapleural pneumonectomy and chemo to treat his pleural mesothelioma.
“It had become almost impossible for me to sleep, and I began using mild medication to help,” Michael shares with us. “My thoracic surgeon recommended I speak with a psychiatrist. [They] explained how trauma to the body interacts with brain function, which can result in a loop effect causing more pain and stress.”
Common Questions About Palliative Treatment
- What is the difference between palliative and curative mesothelioma treatment?
-
Palliative treatment focuses on helping you feel better, managing symptoms like pain or trouble breathing. Curative treatment, on the other hand, tries to remove or destroy the cancer and stop it from coming back. While palliative care can use curative treatments like immunotherapy and surgery, the aim for this use of those therapies is to help improve your comfort and quality of life while undergoing other treatments to fight the cancer.
- Does insurance cover palliative care?
-
Yes, most insurance plans cover palliative care for mesothelioma. Coverage includes private insurance, Medicare and Medicaid. Coverage depends on your plan and the type of care you need, so make sure to check with your insurance provider. You can also talk to our Patient Advocates to help you understand what’s covered and what you may have to pay for out of pocket.
- Can I receive palliative care at home?
-
Yes, many types of palliative care for mesothelioma can be provided at home. Home-based care may include help with pain management, breathing support, nutrition and mobility. It can also reduce the need for hospital visits and help you stay more comfortable in your daily routine. Your doctor or care team can help set up in-home services that match your needs and insurance coverage.
- What should I discuss with my doctor before starting palliative care?
-
Before starting palliative care for mesothelioma, talk to your doctor about the symptoms that bother you the most, like pain or trouble breathing. Ask what treatments can help you feel better and what side effects to expect. You should also talk about your goals, like wanting to stay active or spend more time at home. Ask where you can get care, how often you’ll need it and if your insurance will help pay for it. Also, ask how your palliative care can work with other treatments and how it might affect you in the long run.







