When I was diagnosed with malignant pleural mesothelioma my specialist told me extrapleural pneumonectomy surgery with heated intrathoracic chemotherapy, or HITHOC, was the best course of action for my case. I said, ” I want you to get everything you can see, everywhere you think it might be hiding and everywhere you think it might go.” He was visibly relieved when I told him that.
Mesothelioma Surgery
Mesothelioma surgery removes tumors in the heart, lungs or abdomen. This approach alleviates symptoms and can extend life. Procedures such as pericardectomy and pleural decortication focus on specific regions. Less invasive techniques speed up recovery and improve results.
What Are the Surgical Options for Mesothelioma?
Surgical options for mesothelioma include extrapleural pneumonectomy, pleurectomy/decortication and peritonectomy. These tumor-removing surgeries cut out as much cancer as possible.
Palliative surgeries treat fluid buildup around the lungs or abdomen. The goal of any surgery is to help you feel better and live longer.
Key Facts About Mesothelioma Surgery
- Mesothelioma surgery can improve a patient’s prognosis, extend survival and improve overall quality of life.
- About 27.6% of pleural mesothelioma patients received surgery between 2004 and 2020, according to the National Cancer Database.
- About 50% of peritoneal patients who undergo cytoreductive surgery with heated chemotherapy live longer than 5 years.
- Pain and swelling around the incision are the most commonly reported complications of surgery.
Diagnostic surgical procedures play a pivotal role in confirming the type and stage of mesothelioma. Thoracoscopy, also called video-assisted thoracoscopic surgery, is the most accurate diagnostic test for pleural mesothelioma. A laparoscopy is the best for diagnosing peritoneal mesothelioma.
To diagnose and treat mesothelioma, you might undergo multiple surgeries. Your doctor’s recommendations will vary depending on the type and stage of your disease.
There’s two categories of surgery we can offer pleural mesothelioma patients. Palliative surgery’s goal is to improve quality of life. The goal of curative surgery for mesothelioma is to remove all the disease that can be seen with the naked eye.
Pleural Mesothelioma Surgery Options
Pleural mesothelioma has the most surgical options. However, these procedures are less effective than surgeries for peritoneal mesothelioma patients.
About 15% to 20% of patients with pleural mesothelioma qualify for surgery. Specialists will recommend the treatment for mesothelioma that best meets your needs and goals.
Multimodal therapy combines major, tumor-removing surgery with other treatments, including radiotherapy and chemotherapy. This aggressive treatment approach can extend life expectancy.
Curative Surgeries for Pleural Mesothelioma
The most aggressive surgeries for pleural mesothelioma include pleurectomy and decortication as well as extrapleural pneumonectomy. Surgeons use more aggressive surgeries on people diagnosed in the early stages of mesothelioma. When deciding between pleurectomy versus pneumonectomy, surgeons will consider your unique medical needs and preferences.
- Extrapleural pneumonectomy: An EPP is an aggressive procedure that removes an entire lung, the lining around it and nearby lymph nodes. Benefits include improved symptoms and median survival after EPP is about 15 months.
- Partial pleurectomy: Also known as debulking surgery, a partial pleurectomy aims to remove as much tumor tissue as possible when the tumor can’t be completely removed. The partial pleurectomy involves opening the chest cavity and removing the outside of the pleural layer that lines the chest wall and lungs. It removes all visible cancerous tissue.
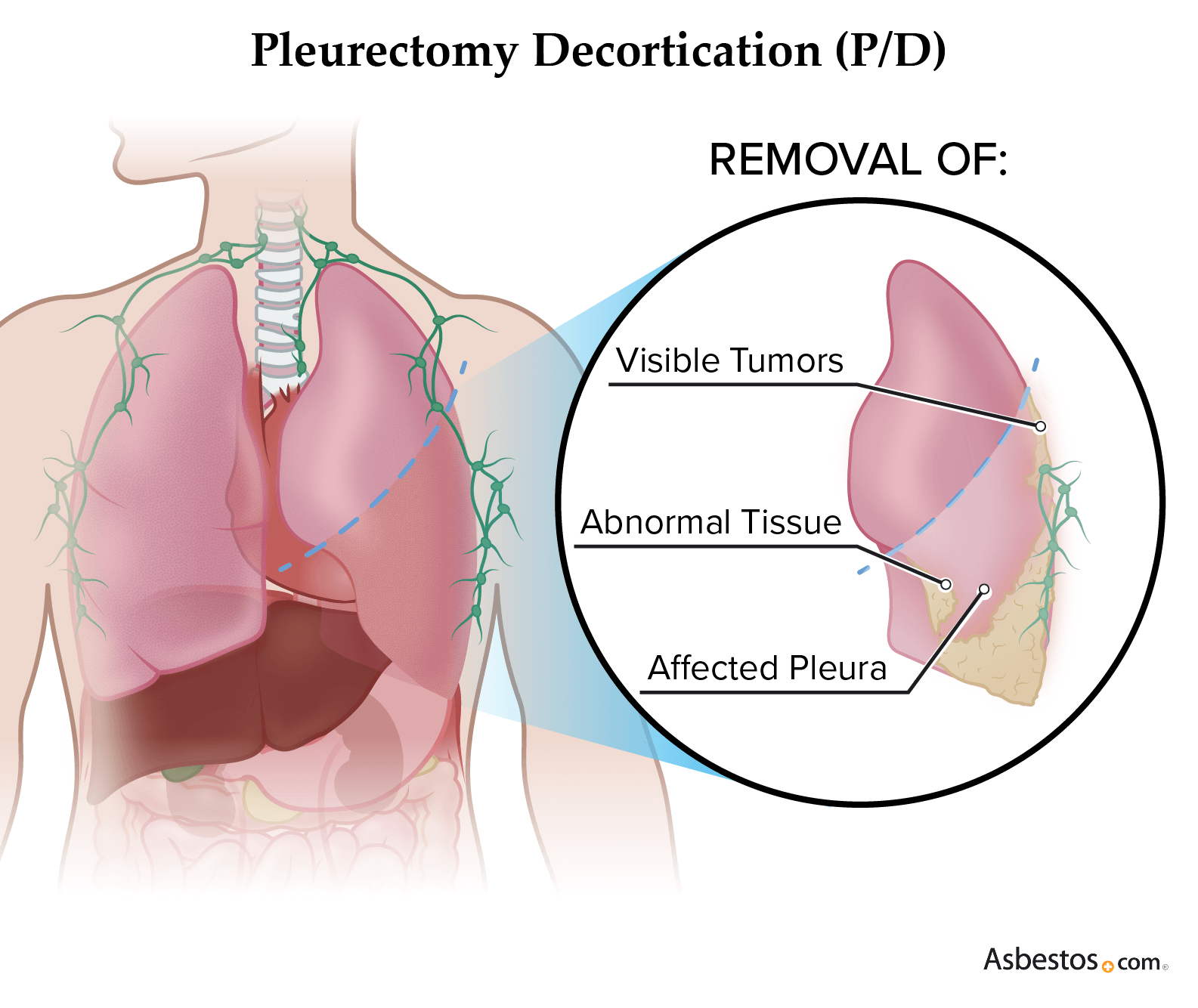
- Pleurectomy and decortication: P/D removes the pleural lining around the lungs and all visible tumors. They scrape the surface of the diseased lung rather than removing the organ. P/D has a median survival of 22 months.
These surgeries may take several hours to complete, and recovery time varies depending on the procedure. A 2024 long-term survival analysis published in the journal Clinical Lung Cancer found the pleurectomy and decortication patient group had 10-year overall survival rates of 16%, significantly higher than any other group.
Palliative Surgeries for Pleural Mesothelioma Patients
Palliative procedures help control symptoms and improve quality of life. They may be an option for people at all stages of pleural mesothelioma, on their own or in conjunction with curative treatment.
- Pleurodesis: Drains fluid buildup between layers of the pleura lining the lungs. In a talc pleurodesis, a surgeon uses medical-grade talc during the procedure to cause the lung to stick to the chest wall, decreasing the likelihood of the pleural fluid returning.
- PleurX catheter placement: Surgical placement of a small silicone catheter, called a PleurX, allows the patient to drain pleural fluid at home every two to three days without having to undergo another thoracentesis. A home health nurse will teach the patient how to perform this drainage.
- Thoracentesis: A doctor can drain pleural fluid through a hollow needle during a thoracentesis to relieve pressure and make it easier to breathe. Removing the fluid reduces pressure on the chest and lungs and also offers more space for the lungs to expand.
Patients not eligible for more aggressive mesothelioma treatment options may elect these palliative surgeries, and some people live longer thanks to these surgeries. Risks include pain at the incision site and infection.
Peritoneal Mesothelioma Surgery Options
The most effective and aggressive surgery for peritoneal mesothelioma is cytoreductive surgery with heated chemotherapy, known as HIPEC. Approximately 50% of peritoneal mesothelioma patients qualify for tumor-removing surgery.
Surgeries for Peritoneal Mesothelioma
- Cytoreductive surgery: Tumor-removing surgery can have palliative benefits, reducing symptoms. It can also help some patients achieve remission. This type of surgery aims to remove as much cancerous tissue as possible. Cytoreductive surgery is a broad surgical approach during which specific procedures may be done.
- Components of cytoreductive surgery: Surgical procedures like omentectomy and peritonectomy are done during cytoreductive surgery and remove specific types of tissues from the abdominal cavity. Peritonectomy removes diseased parts of the peritoneum. An omenectomy removes an apron of the peritoneum called the omentum. Peritonectomy can be paired with heated chemo or HIPEC applied directly in the abdomen. Omenectomy can improve the effectiveness of heated chemo.
- Palliative surgeries: Paracentesis is commonly performed to drain excess fluid buildup. To avoid the need for multiple paracenteses, sometimes small, flexible tubes or indwelling peritoneal catheters (tunnel or PeritX) are inserted to drain fluid. They can be left in place, allowing you to manage ascites at home.
Doctors perform procedures like peritonectomy and omentectomy to remove as much tumor tissue as possible during cytoreductive surgery. Benefits include improved symptoms and longer survival with cytoreductive surgery and HIPEC.
Repeat HIPEC with surgery patients live 67.7 months or 5.6 years, according to a 2022 study published in Annals of Surgical Oncology. Risks include infection, digestive issues, excessive bleeding and constipation.
I think the best treatment for peritoneal mesothelioma is a combination of HIPEC or the hypothalamic interpersonal chemotherapy as well as what we call a cell reductive procedure. Which includes the peritonectomy procedure.
Pericardial Mesothelioma Surgery Options
Surgeries for pericardial mesothelioma involve removing affected tissue or draining fluid buildup. These procedures have varying success rates and tend to have higher risks of serious complications.
- Pericardiectomy: Removes as much cancerous tissue as possible from the heart lining, or pericardium. It can relieve symptoms such as difficulty breathing, chest pressure, heart palpitations and fatigue.
- Pericardiocentesis: Similar to thoracentesis and paracentesis, but the fluids are removed from around the heart rather than the lungs or abdomen. Doctors treat recurrent pericardial effusions with repeat pericardiocentesis procedures.
These procedures can improve quality of life and relieve symptoms like shortness of breath, coughing and chest pressure. Risks include infection, abnormal heart rate and cardiac arrest. After you get home from surgery, you should contact your doctor if draining from the incision increases or you notice chest pain or severe symptoms.
In pericardial mesothelioma patients, symptoms are often the result of inflammation of the pericardium (pericarditis) and buildup of fluid (pericardial effusion). It’s important to treat these conditions early because they can lead to deadly complications if untreated.

Join our upcoming webinar where two leading mesothelioma specialists explain how they tailor treatment plans to each patient’s needs.
Sign up nowSurgery for Testicular Mesothelioma
The most common treatment for testicular mesothelioma is inguinal orchiectomy, a surgery to remove one or both testes along with the spermatic cord. The risks include bleeding, infection, swelling and pain.
A urologic oncologist, a specialist in cancers of the urinary tract and reproductive system, typically performs the surgery. The surgeon may also perform a lymphadenectomy to remove nearby affected lymph nodes.
Survival rates are higher among testicular patients compared to pericardial patients. Most patients undergo surgery and nearly 49% of them survive 5 years after diagnosis, with 33% surviving 10 years.
The statistics about surgery are based on clinical research and apply only to people diagnosed with different types of mesothelioma cancer. These statistics do not reflect other surgery stats for the population at large.
Who Is Eligible for Mesothelioma Surgery?
You may be eligible for surgery if you’re in good overall health and your doctor is confident you can recover from potential complications. You may not qualify if you have the sarcomatoid cell type, late-stage cancer or certain preexisting conditions. It’s important to speak with a surgical specialist to determine if you meet the criteria.
- Cancer stage and cell type
- Cardiac health
- Comorbidities like high blood pressure and diabetes
- Overall health
- Past surgical history
- Smoking status
Eligibility for surgery is thoroughly vetted during a surgical consultation, where the surgeon and the surgical team review your medical history, imaging scans and biopsy results. Surgical consultations allow you to meet with the surgeon and their team to discuss everything about the procedure, including preparation and recovery.
If you qualify for surgery, you also may be able to join a mesothelioma clinical trial of other treatment options. Mesothelioma surgeons can offer patients the opportunity to participate in clinical trials to investigate optimal therapies to combine with surgery.
Benefits of Mesothelioma Surgery
Benefits of surgeries for mesothelioma include longer survival and improved symptoms. Pleural surgery reduces chest pain and improves breathing and coughing. Peritoneal surgery improves abdominal pain and swelling as well as digestive symptoms such as constipation. Although mesothelioma is often considered a terminal illness, surgery offers the potential for long-term survival in select cases.
- Improved prognosis and extended survival: Mesothelioma surgery can extend survival significantly when performed at an early stage. P/D and EPP offer similar survival outcomes. EPP has a median overall survival of 12 to 22 months compared with 13 to 29 months for P/D. About 24% of patients with early-stage mesothelioma live at least 5 years, and most of these patients undergo multimodal treatment with surgery.
- Improved quality of life: Surgery can alleviate symptoms such as chest pain, difficulty breathing and fluid buildup in the chest cavity.
Advances in surgical techniques, such as minimally invasive surgery and robotic surgery, have improved outcomes and reduced postoperative complications. Benefits of robotic surgery include reduced blood loss, less pain, reduced postoperative recovery time and less stress on the remaining lung after an EPP procedure.
Risks and Possible Mesothelioma Surgery Complications
The most common complications of mesothelioma surgery are pain and swelling around the incision. This usually gets better over time, but it depends on the extent of the surgery.
Aggressive surgery can potentially remove mesothelioma completely. However, there’s a risk that some cancer cells left behind can grow and divide to form new tumors. Chemotherapy is used in conjunction with surgery to eliminate remaining cancer cells to prolong survival.
- Bleeding: After chest surgery, some patients may cough up a small amount of blood. This usually disappears after a few days. Some patients may also have a small amount of bleeding from the incisions.
- Cardiac complications: Mesothelioma surgeries in the chest cavity pose the risk of cardiac complications. The most common risk is atrial fibrillation or cardiac arrhythmia (irregular or abnormal heartbeat).
- Dry cough: A dry cough after lung surgery is usually the result of irritation of the remaining lung. Once the remaining lung recovers, your dry cough will disappear. This may take several weeks.
- Fatigue: Patients may feel fatigued from the stress of an invasive procedure. Failing to get good nutrition and plenty of rest to restore the body’s energy levels can intensify fatigue.
- Infection: If you feel warm, flushed, chilled or dizzy, take your temperature with a thermometer. If you’re running a fever or have a port or catheter and notice redness, swelling, tenderness or pus around the wound, call your doctor.
- Pain after surgery: Pain may come from your incision or may radiate toward your back or your belly. Alternatively, you may feel tingling, numbness, pins and needles, bloating or a sensation of electric shock.
- Pneumonia: The most common complication after major chest surgery is pneumonia. The best way to avoid pneumonia is to breathe deeply, cough up secretions and walk immediately after surgery.
It’s important for surgical candidates to speak with their surgeons about the risks and benefits of different procedures. If you have any questions about complications or feel any effects are worse than they should be, call your doctor right away. Addressing complications quickly is important throughout the recovery process.
Mesothelioma Surgery Recovery
Each patient has a different mesothelioma surgery recovery process depending on the surgery they had, their overall health and whether any complications arise. How long it takes you to recover and the amount of pain you feel will depend on the extent of your procedure.
Your surgeon can help you develop a recovery and pain management plan to cope with the discomfort you experience after surgery. Before you leave the hospital, you’ll get a prescription for oral pain medication and more information about the recovery process.
The recovery process varies for people who undergo chemotherapy or radiation therapy after surgery. Doctors often tailor multimodal therapy plans around each patient’s health. Some patients may receive additional therapies soon after surgery, while other patients may require several weeks of recovery.
Recovery may take longer for patients who undergo aggressive surgeries such as the EPP. When we asked Dr. Jacques Fontaine, thoracic surgeon and director of the Mesothelioma Research and Treatment Center at Moffitt Cancer Center, about the EPP surgery, he said the EPP “is a tough recuperation that can take 3 to 6 months.”
Your surgical team will provide guidance to help you understand how to prepare for the recovery process at home. They’ll also schedule follow-up appointments for imaging scans to observe the outcome of the surgery. Patients should be careful to follow any instructions and attend all medical appointments to help their recovery.

Filled with thoughtful items to bring comfort and encouragement while undergoing treatment.
Get Your Free KitWhat to Do if You’re Considering Mesothelioma Surgery
Before undergoing surgery for mesothelioma, talk to your surgeon to make sure you understand the risks and benefits of the procedure. Ask questions about how the procedure may affect your body, quality of life and lifespan to make an informed decision about mesothelioma surgery.
- What surgical option is best for me?
- What are the benefits of this procedure?
- What risks could I face if I choose to have this surgery?
- What can I do to reduce my risks of complications?
- How can I best prepare for surgery and recovery?
You should prepare for surgery based on the guidelines your surgical team provides. Planning for the recovery process involves building a good support team at home and making sure your caregivers are prepared to help. Talk to your doctors about follow-up appointments to see if your surgery was successful.
Common Questions About Surgery for Mesothelioma
- Can mesothelioma be removed with surgery?
-
Yes, aggressive surgeries attempt to remove early-stage mesothelioma completely, but some microscopic cancer cells are often left behind. Chemotherapy and radiation may help to kill the remaining cancer cells.
- How will I know if I’m eligible for mesothelioma surgery?
-
You can book a surgical consultation with a thoracic surgeon to learn about your eligibility. They’ll review your medical records, imaging scans and pathology report to determine if surgery is appropriate.
- How successful is surgery for mesothelioma?
-
About 24% of early-stage mesothelioma patients live at least 5 years after surgery. An EPP and P/D have a risk of failure with mortality rates around 11% and 3.1%, respectively.
- What is the prognosis for mesothelioma surgery?
-
For early-stage mesothelioma patients who undergo aggressive surgery, the prognosis can be more favorable compared to those with advanced-stage disease. Surgery is often part of a multimodal treatment approach, and other therapies impact the prognosis as well.
- Will I need additional treatments such as chemotherapy or radiation therapy following surgery?
-
Doctors may recommend chemotherapy to kill any remaining cancer cells after surgery and radiation to prevent local recurrence. These treatments improve the chance of long-term survival in combination with surgery.











